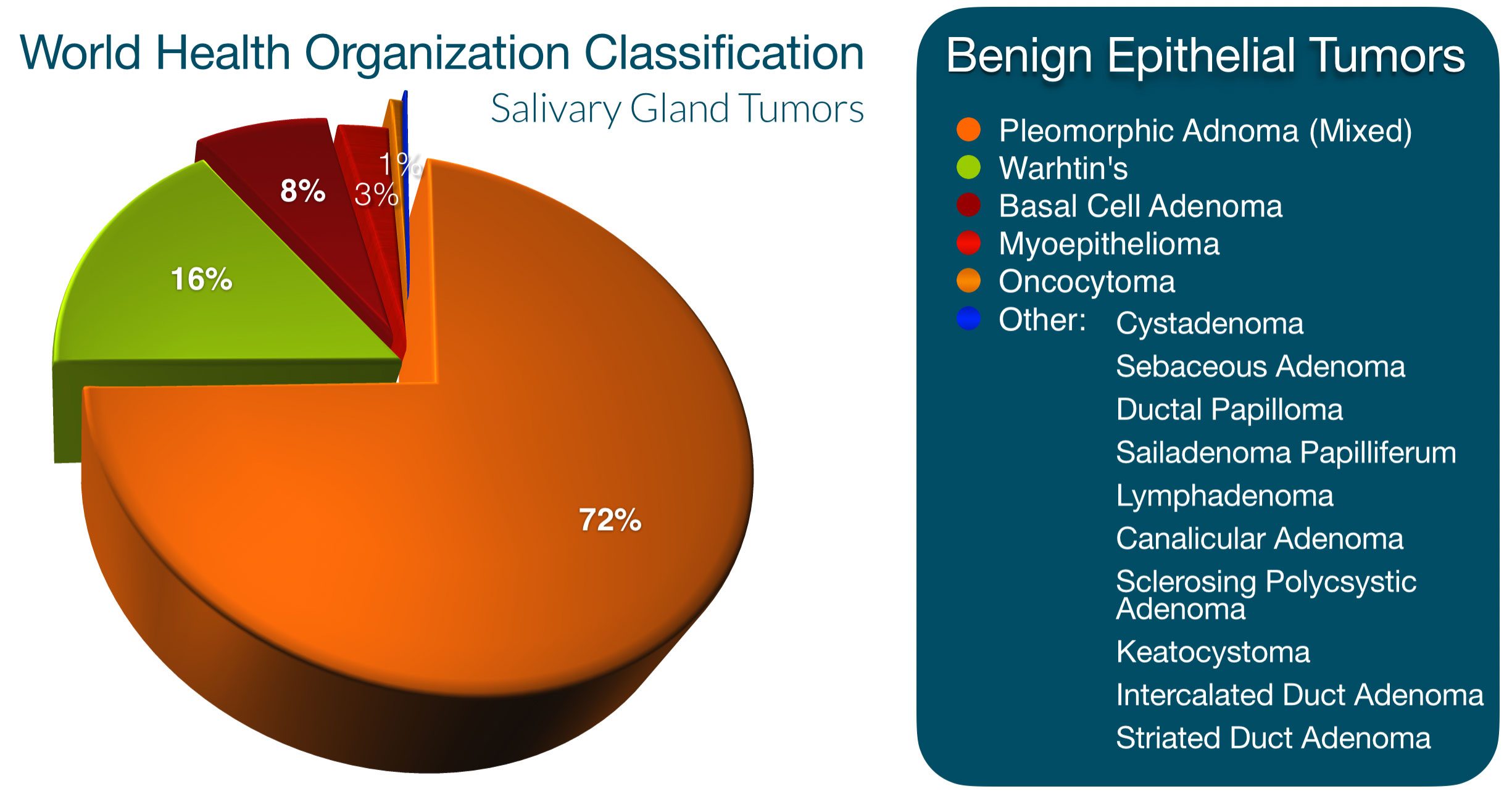
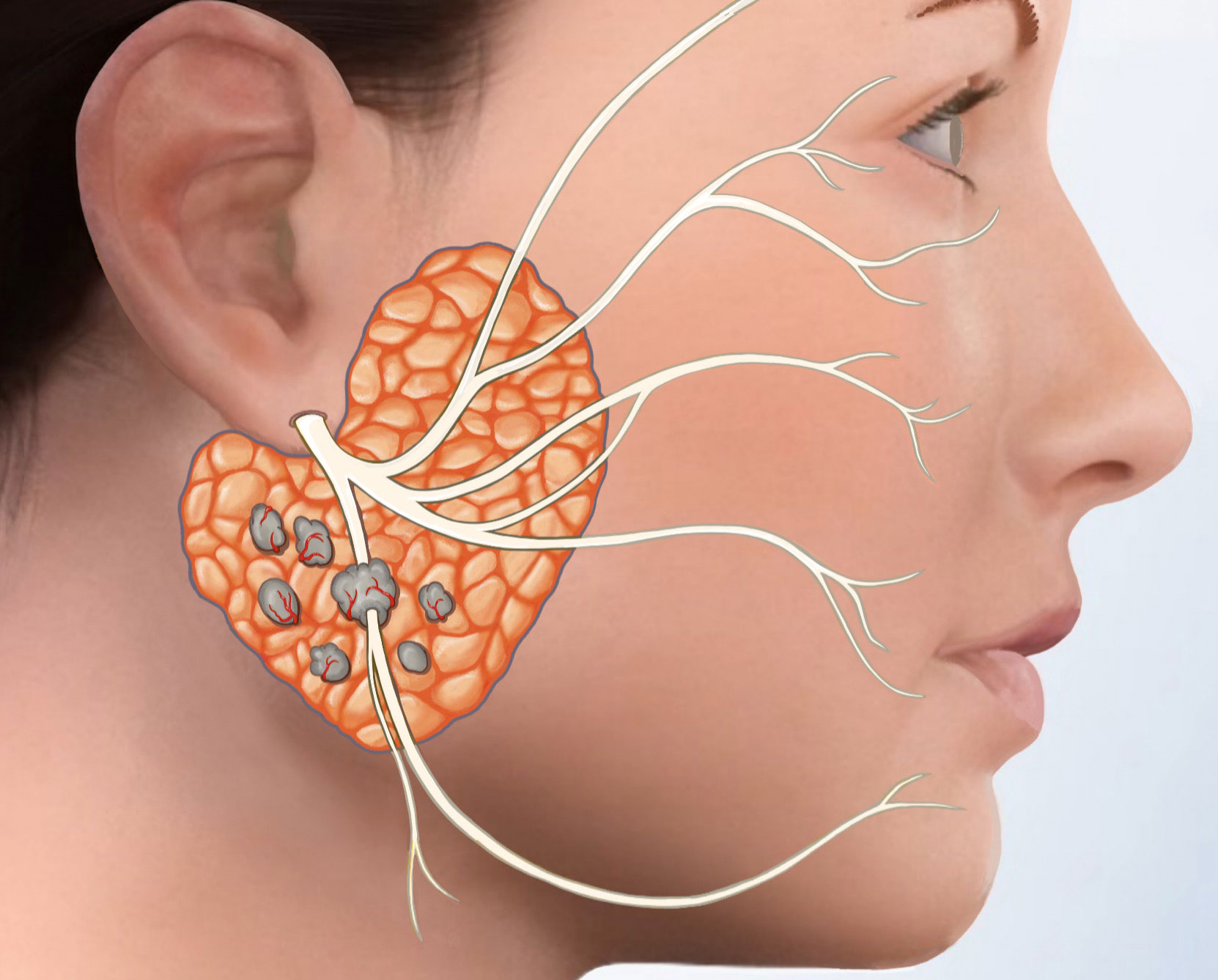
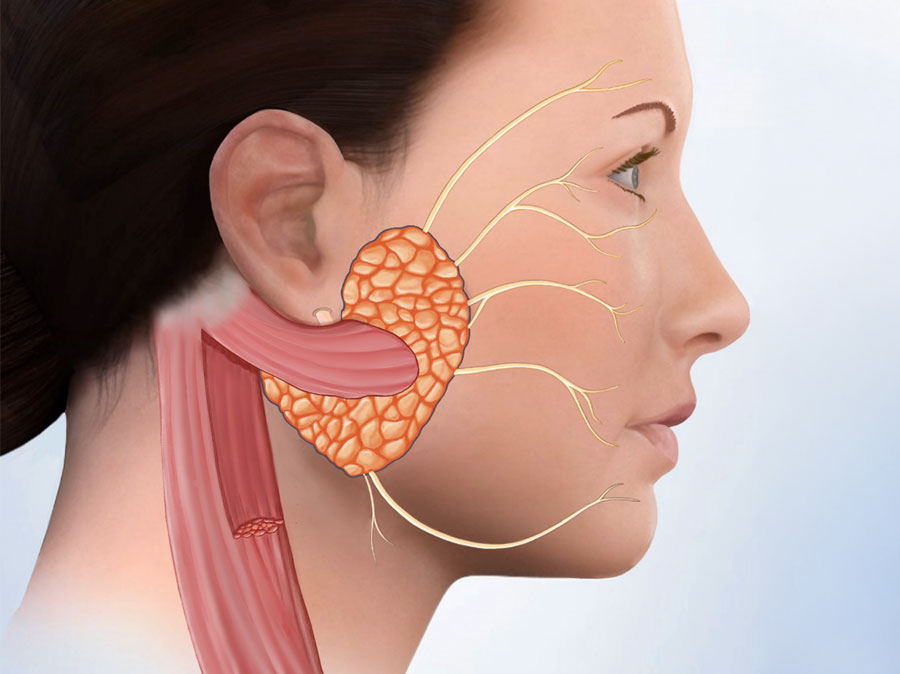
Pleomorphic adenoma (PA) is an enigmatic tumor with a variety of names including benign mixed tumor & adenoma multiforme. It is one of 15 benign epithelial tumors of the salivary glands, and in fact the most common benign tumor of the salivary glands, comprising roughly 50% of all salivary gland tumors. More then 80% of PAs occur in the parotid gland, although they can occur in any of the salivary glands, including unusual locations such as nasal cavity, back of tongue, palate and breathing tube. They can occur at any age but are found most often in women between the ages 40 and 60.
UNDER THE MICROSCOPE
Pleomorphic adenoma’s name is comes from the fact that this odd tumor is made of both epithelial component (the internal lining of the salivary gland) and mesenchymal component (the cells in between the linings) in all of these tumors. The proportion of each component can be different in each person. The epithelial component can form tube-like or solid structures and the in-between areas can contain muscle cells along with cartilage, or rarely bone like formations. Pleomorphic means various distinct forms.
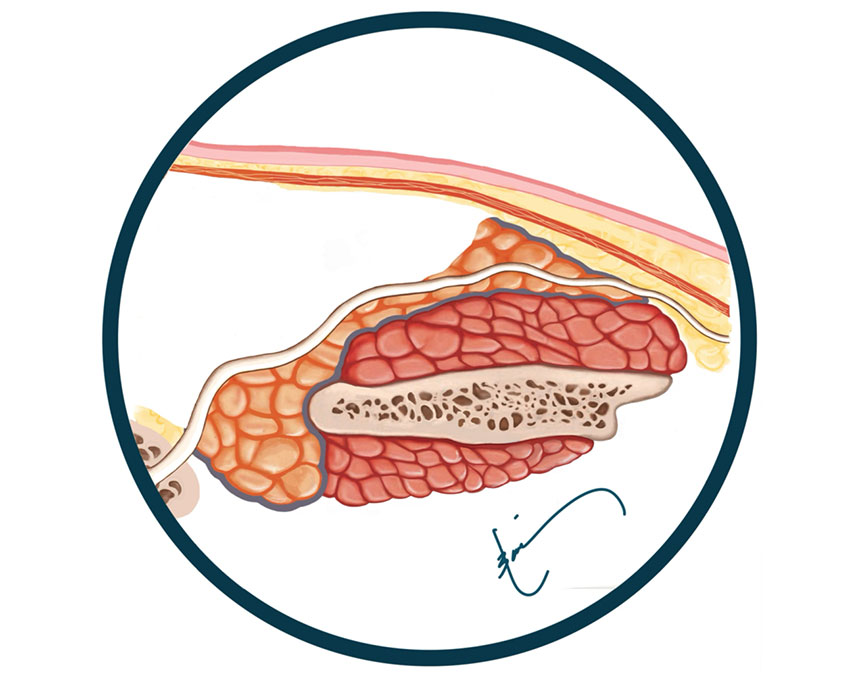
CAPSULE
The covering or capsule of Pleomorphic adenoma is also very odd. It can be thick in some areas, very thin in others, and even completely absent at times. As the tumor grows it seems to stretch out the capsule causing some areas to get thinner and ultimately some areas to break open the covering and therefore have no capsule at all. Smaller tumors tend to have thicker capsules, which is yet one more reason to remove a pleomorphic adenoma at an earlier stage. As such the capsule can have some interesting characteristics:
- Thick Capsule – brown covering of the pink tumor
- Thin Capsule
- Incomplete or Absent Capsule – tumor without a covering
- Capsule Penetration – causes bulging of the tumor
- Pseudopods – little legs that stick out of the tumor
- Satellite Nodule
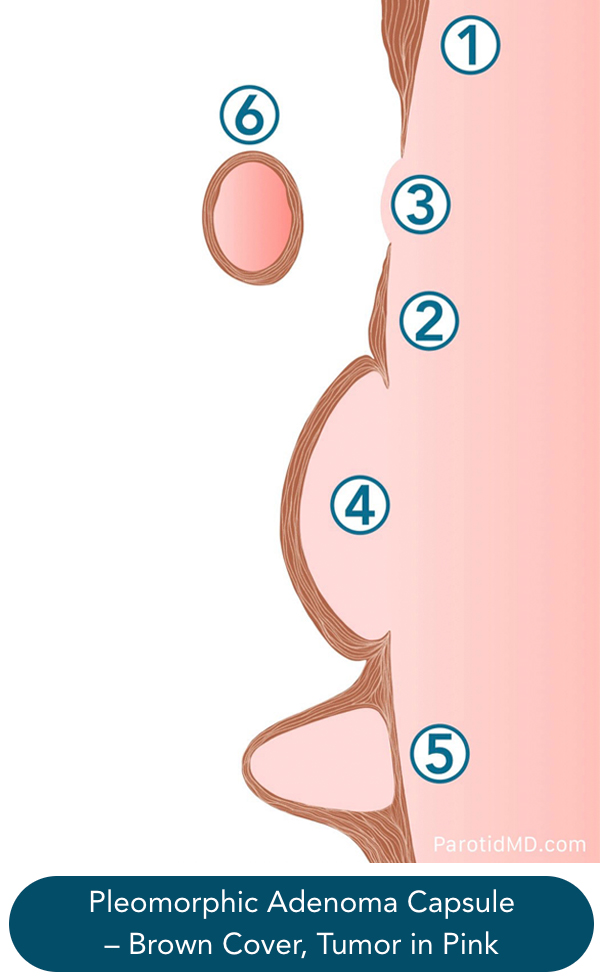
The incomplete capsule can occur from as little as 4% of the surface of the tumor to as high as 28% in some tumors. The greater the area of thin capsule and incomplete capsule the greater the chance that the tumor may rupture or burst open in the process of being removed. This can lead to a recurrence of tumor years later. Again, the experience of the surgeon is of utmost importance in minimizing the risk of rupture happening.
Satellite nodules are fortunately extremely rare. Pseudopods or little tumor legs can cause a problem because if the surgeon is not cautious and cuts these while removing a tumor then that small piece of tumor can grow in time to become a large tumor.
DIAGNOSIS OF PLEOMORPHIC ADENOMA
Pleomorphic adenomas are generally slow growing, the borders are very distinctive and they are mobile (easily moved under the skin). This may make one feel that the history of slow growth and physical ndings is enough to tell us that the tumor we are dealing with is benign. Unfortunately, this is not always the case. Most parotid cancers are discovered in the earlier stages when they are small and have not set out deep roots, so that they are mobile. The treatment of non-pleomorphic adenoma benign tumors requires only removal of tumor. Pleomorphic adenomas need to be removed with an bit of extra salivary gland tissue around it to prevent return or recurrence of tumor. While low grade cancers require bigger amounts of normal salivary tissue to be removed around the, and aggressive cancer require even more extensive removal of parotid tissue along with removal of neck lymph nodes. So knowing what type of tumor you are dealing with allows you to be prepared and your surgeon to have a concise treatment plan.
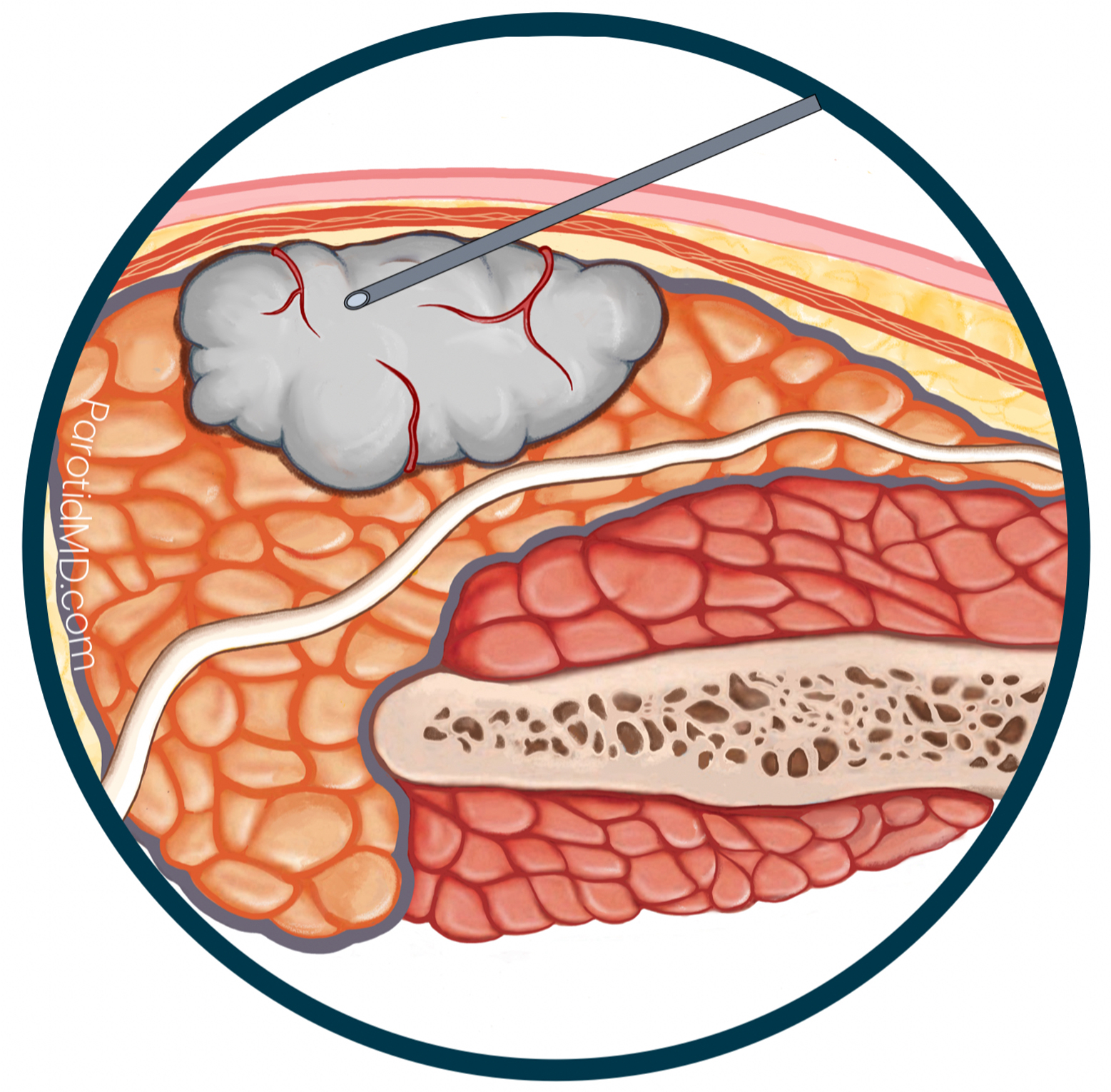
Needle biopsy of parotid tumors is a very accurate way of identifying the type of tumor you are dealing with. At the CENTER we perform ultrasound guided needle biopsy of almost all parotid tumors, and for our patients that live in other cities or countries we help you arrange for a biopsy. Needle biopsies of salivary tumors are accurate in about 95% of cases; this means in roughly 5% the needle biopsy results that may indicate a benign tumor will be found to be not benign or a different kind of tumor. This is where your surgeons experience is very important. During surgery if Dr. Larian sees signs that the tumor is more such as areas of rmness in the tumor, invasion of adjacent tissue, or involvement of nerves then he will send the tumor to be examined by a pathologist immediately during surgery to give him more information, so that he can do the correct surgery.
RECURRENT PLEOMORPHIC ADENOMA
Recurrent PA is a misnomer, in that it is not a reoccurrence of a tumor but rather regrowth of an incompletely removed tumor; it has now grown large enough to be visible. PA has a low rate of recurrence when treated by the appropriate surgery (1-4%). The three main mechanisms of recurrence are (1) rupture of the tumor and spillage of tumor cells into the eld or surgery (2) amputation of the pseudopods & (3) satellite lesions (which is more rare). In all of these scenarios some tumor cells are left behind, which in time (usually years) grow to show themselves.
Tumor Rupture – As discussed in the description of the PA capsule these tumors can have anywhere between 4% to 28% of the surface of the tumor not have a covering (incomplete capsule). These areas are weak and can easily break open.
As the tumor gets larger the capsule gets stretched out and more gaps form, thus increasing the chance of rupture. During the process of removal if the tumor is pressed too hard and breaks open, some of the content (microscopic tumor cells) may spill into the wound thus seeding the surgical eld. If this happens then over the years these small bits of tumor grow larger and larger until they show themselves as multiple tumors that are felt or seen on scans.
Parotid tumors including pleomorphic adenomas are most often sitting adjacent to one or more branches of the facial nerve, as such they need to be very carefully and meticulously separated & manipulated to allow their removal. With experience & patience, the surgeon will be more capable of doing this without rupturing the tumor. It is imperative that your surgeon has extensive experience in treating PAs to have developed an instinct for performing surgery on this delicate tumor in this very strategically important area of your face.
Pseudopod Amputation – If the surgeon gets too close to the tumor, it is possible that they may cut one or more of the little legs (pseudopods) on the surface of the PA. This is the reason the surgery to remove a PA involves removing a small amount of additional parotid tissue around the tumor, so as to stay away from the pseudopods. However in the area where a branch of the facial nerve is immediately close to the capsule of the tumor, it is not possible to remove additional parotid tissue. Despite this the incidence of recurrence is low in the hands of expert surgeons.
Satellite Tumors – The incidence of a separated piece of PA from the main tumor area is fortunately extremely low. Over the last 3 decades I’ve only seen 2 cases of recurrence due to satellite tumors. But generally it can be avoided by getting an appropriate amount of additional parotid tissue around the tumor.
TREATMENT OF RECURRENT PA
The best treatment for recurrent pleomorphic adenoma is surgical removal. These tumors unfortunately don’t resolve on their own without treatment and continually grow. There are also reports that the incidence of transformation into a cancer is higher in recurrent PA. This may be related to the fact when a person has a recurrent PA it means that it was present for a while before first discovered, and then they had surgery to remove it (but not entirely removed) and the tumor cells left behind continued to grow for years & years before being discovered again; which essentially shows that the tumor that we are calling recurrent has been present in the parotid gland of the person for very many years which increases the opportunity for transformation into a cancer.
Treatment of recurrent disease is more complicated because of two reasons: (1) scarring in the area of the parotid due to previous parotid surgery & (2) due to the fact there are usually multiple tumors when a recurrence is found the extent of the surgery has to be more to prevent further recurrence.

Recurrent PA – a few tumors (4)

Multiple Recurrent PAs within the parotid & skin
Rarely, a recurrent PA is found that is a single tumor. On MRI scan or ultrasound not other tumor is found. Even in this scenario, a surgeon with expertise will assume there are more microscopic pieces of PA and remove more of the. surrounding parotid tissue, to be safe.
Role of Radiation Treatment
– Generally speaking when a recurrence is found and there are multiple tumors that have been removed (found in the pathology specimen under the microscope), then it is safe to assume there are more microscopic tumor cells that may not have been visible and still remaining in the area of previous surgery. At times, the recurrence may grow in the skin or muscle next to the parotid gland, or even surround the nerves. All of this will make it impossible to completely remove a recurrent PA, which is why we recommend radiation therapy to the area after surgery to significantly reduce the chance of the tumor coming back again.
CARCINOMA EX-PLEOMORPHIC
Carcinoma ex-pleomorphic adenoma or Ca-Ex-PA makes up roughly 10% of salivary gland cancers. It always arises or transforms from a benign pleomorphic adenoma that has not been removed or has recurred after incomplete surgery. The chance of a benign pleomorphic adenoma transforming into cancer is 1.5% at 5 years and 10% at 15 years, and unfortunately the chance continues to increase in time. The transformation starts in one cell that turns into a cancer. Then that cell starts to rapidly duplicate and get bigger. At first the transformed cancer is small and exclusively inside the capsule of the pleomorphic adenoma. This is designated as non-invasive Ca-ExPA, as the cancer cells are not invading the capsule or covering of the benign tumor. As the cancer grows at some point it starts to eat through the capsule of the tumor, and grow out; when the cancer has grown out less then 1.5 millimeters it is called minimally invasive carcinoma ex-pleomorphic adenoma. It will continue to grow more, and once beyond 1.5 millimeters, it is now called invasive Ca-Ex-PA.
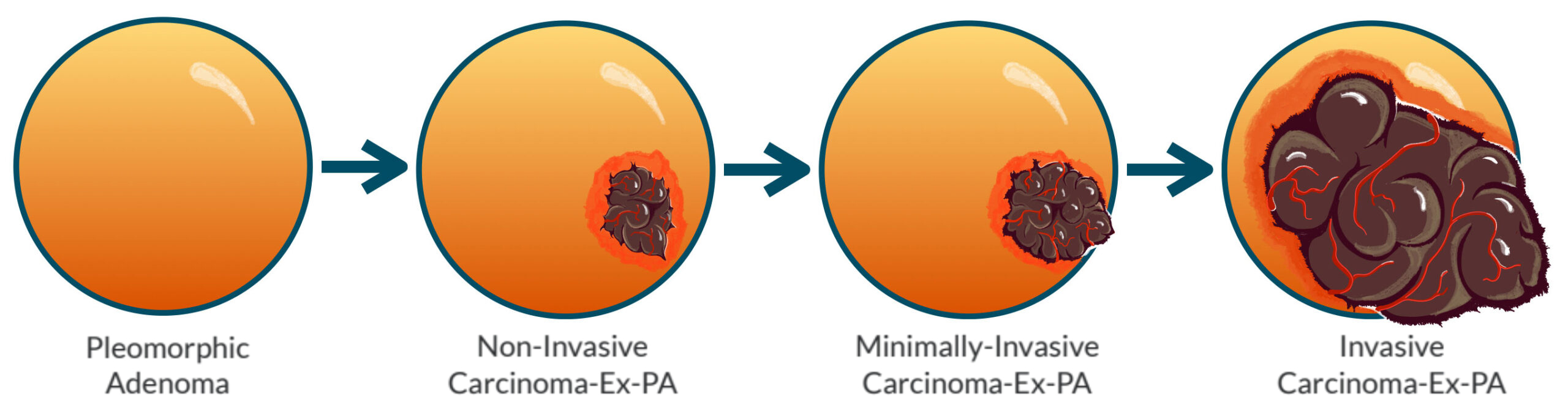
Additionally, carcinoma ex-pleomorphic adenoma can take the form of any of the other salivary cancer, most commonly adenocarcinoma, epithelial-myopithelial carcinoma, or salivary ductal carcinoma. Whatever type of cancer it to becomes, the level of aggressiveness will be similar to that cancer. So if the cancer is diagnosed at non-invasive or minimally-invasive stage and it happens to be a type that is relatively low grade then surgery alone may be adequate as treatment. If the Ca-Ex-PA is invasive, a more aggressive type, or spreads to lymph nodes it will require more involved parotid surgery, lymph node removal followed by radiation therapy, and potentially immunotherapy or chemotherapy. Specialized testing will be done to the cancer once removed to know the exact type, and see if it has specific proteins on it that can be used for immunotherapy (specific targeted therapy).
This is a particularly challenging problem because often times you and your doctor may not know before surgery that the pleomorphic adenoma has transformed. The experience of your surgeon will increase the chance of identifying that the tumor has transformed at the time of surgery, and also be able to address it appropriately. And also know how to plan an optimal treatment for you after surgery.
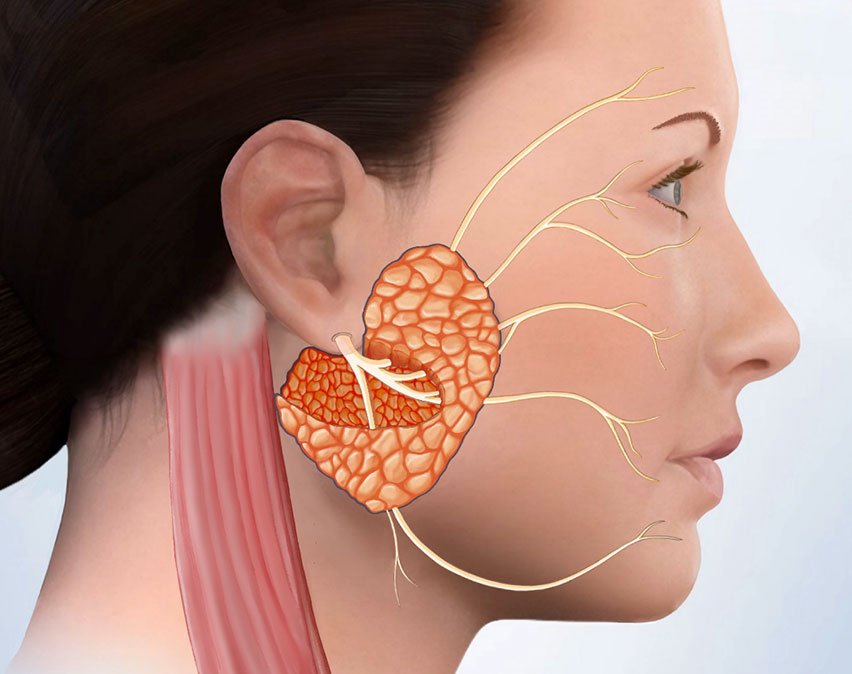
SURGERY FOR PLEOMORPHIC ADENOMA
Surgery is the only effective way to treat pleomorphic adenomas. It was traditionally done by making very large incisions on the face and neck. Dr. Larian and his team have innovated and perfected this surgery and now can treat PAs through the micro-parotidectomy approach, which is the minimally invasive surgery approach. Micro-parotidectomy is an outpatient procedure, with fast recovery (return to work in 1 week), and resumption of exercise in 3 weeks. The pain is minimal and the person can resume a normal diet after surgery. Our patients are encouraged to go for walks several times a day starting the day after surgery.
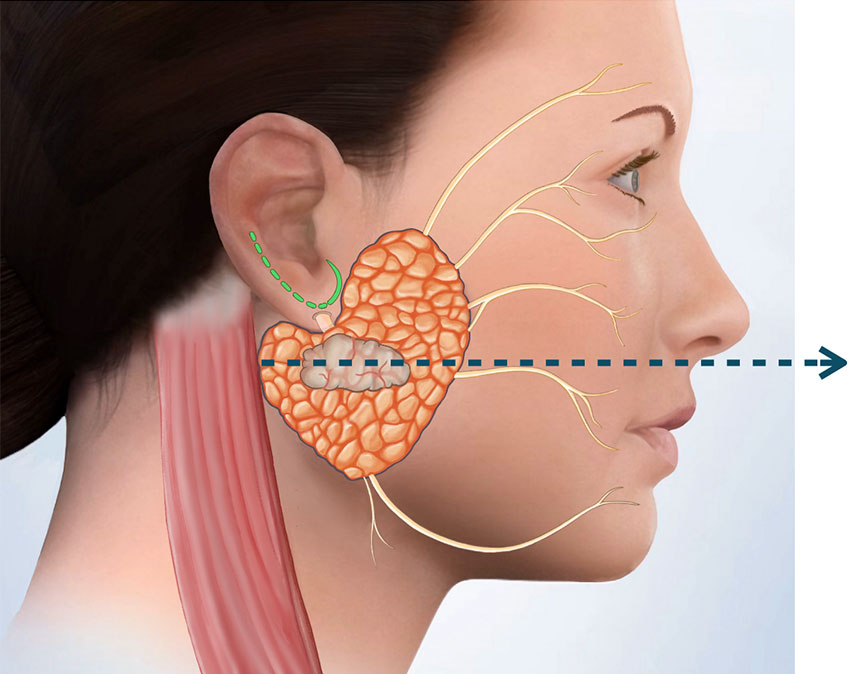
MICRO-PAROTIDECTOMY FOR A SMALL TUMOR
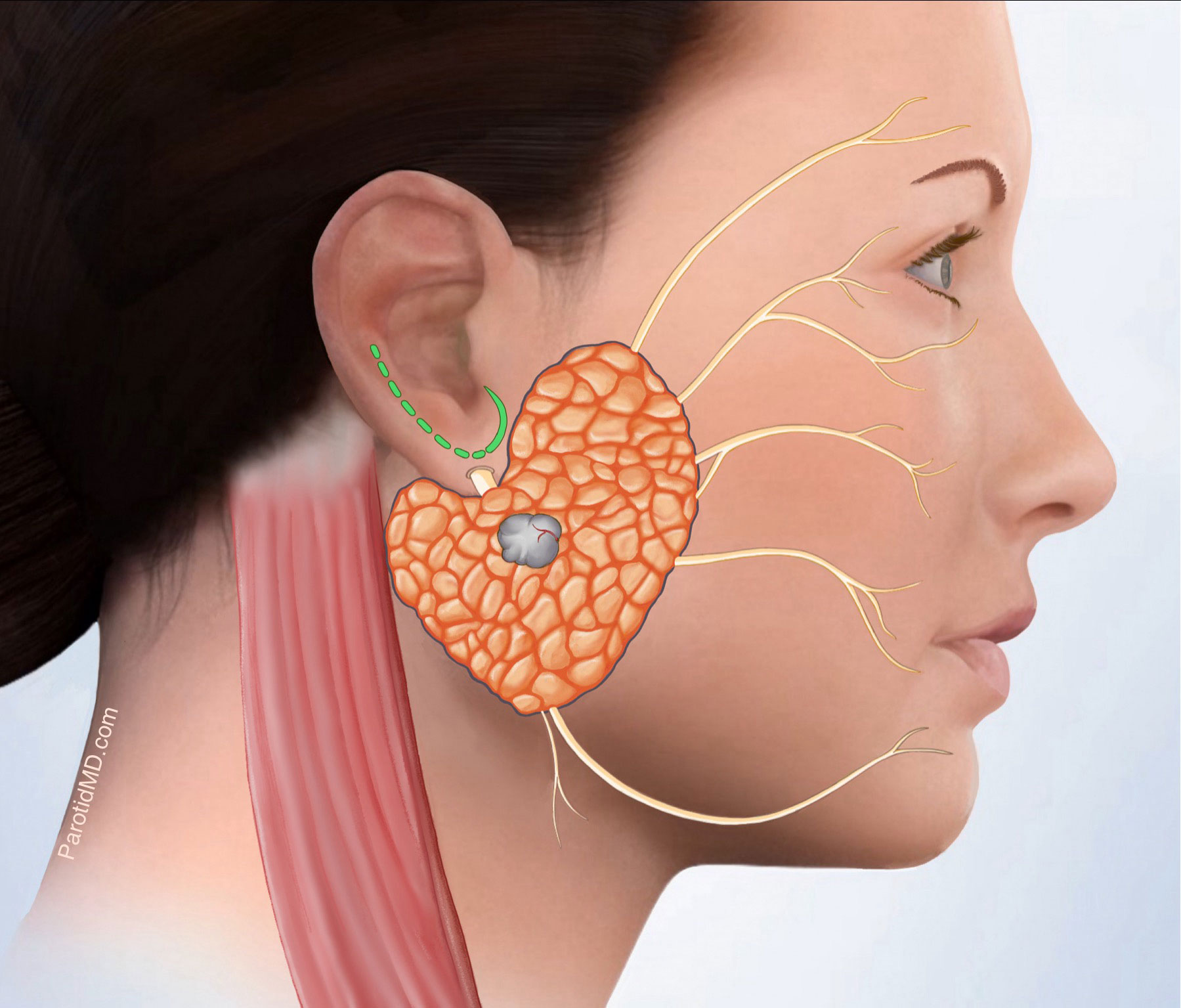
Small parotid tumor (grey)
SCM muscles & facial nerve branches
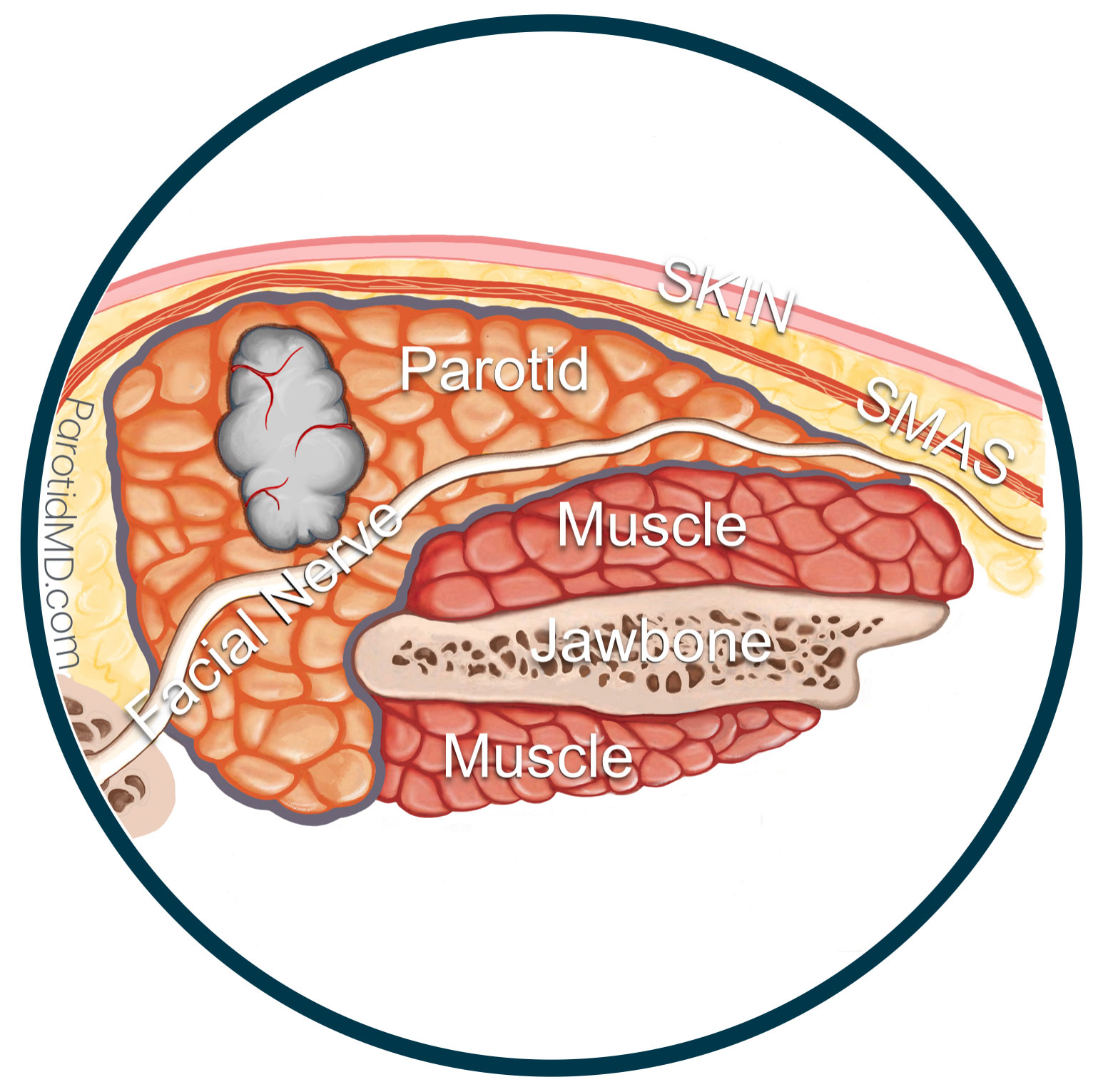
Cross-section of parotid & tumor
Facial nerve (white) going through parotid
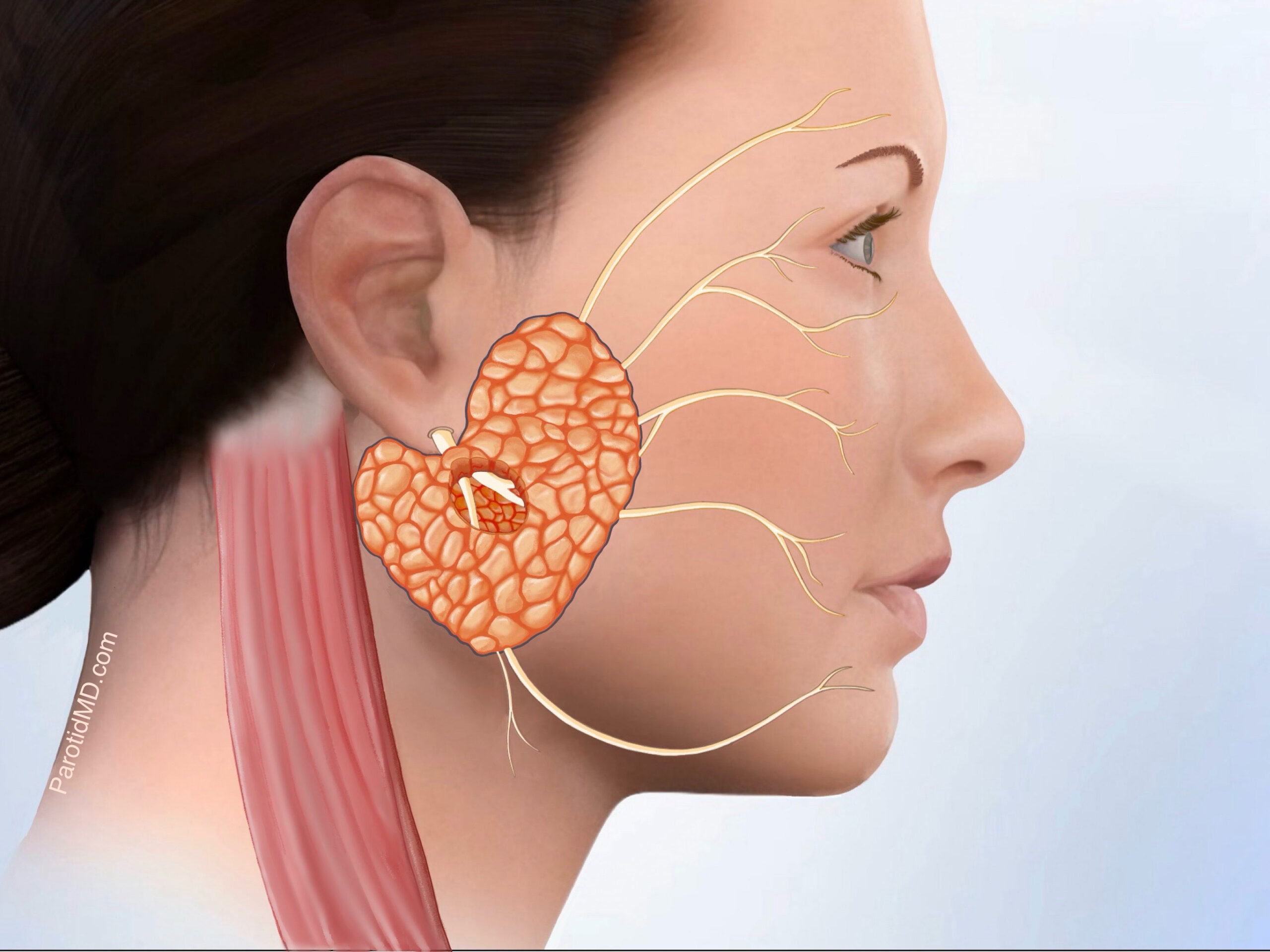
Facial Nerve branches in the area of tumor
identified. Tumor removed with a small cuff
of normal parotid tissue.
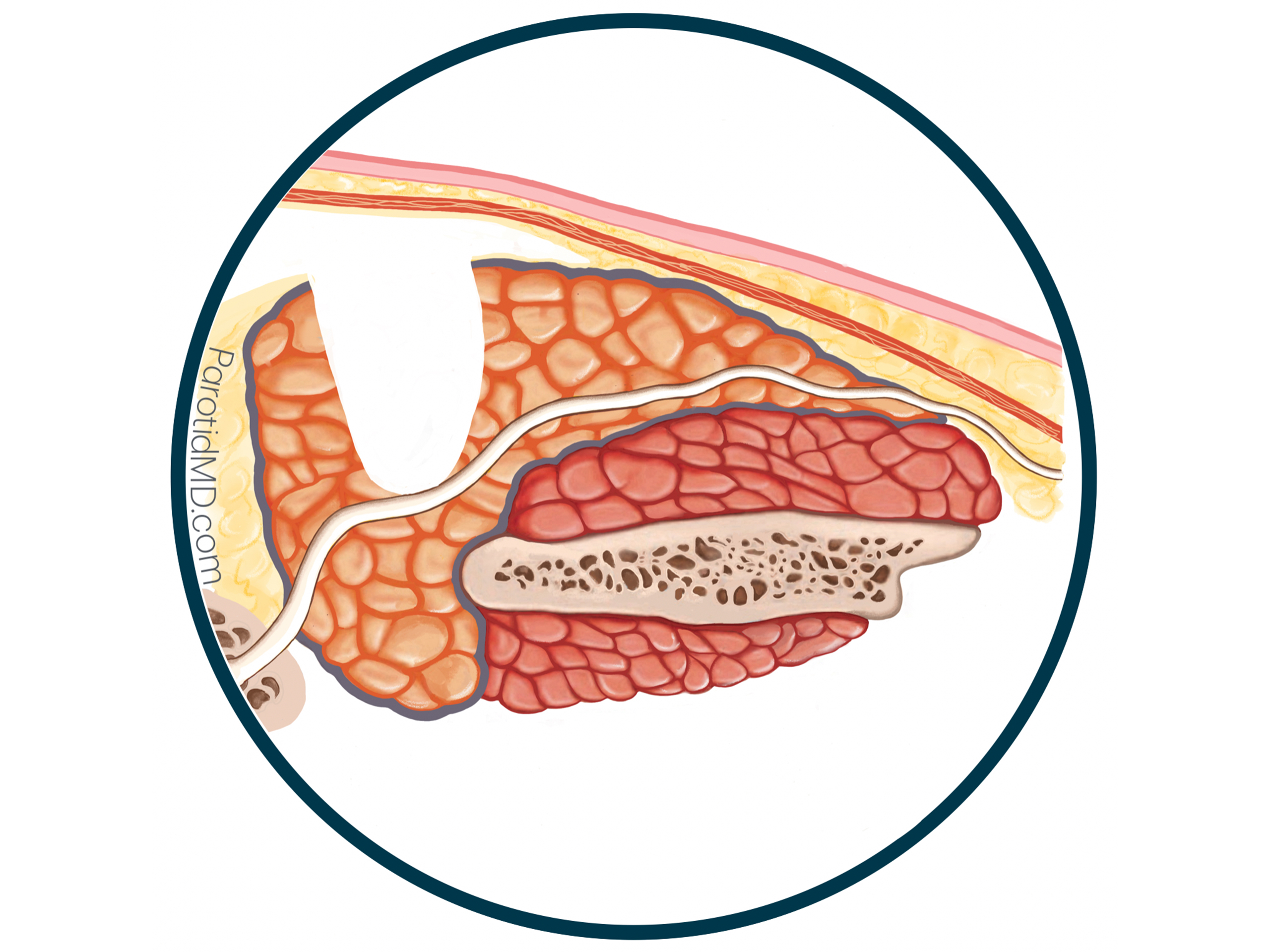
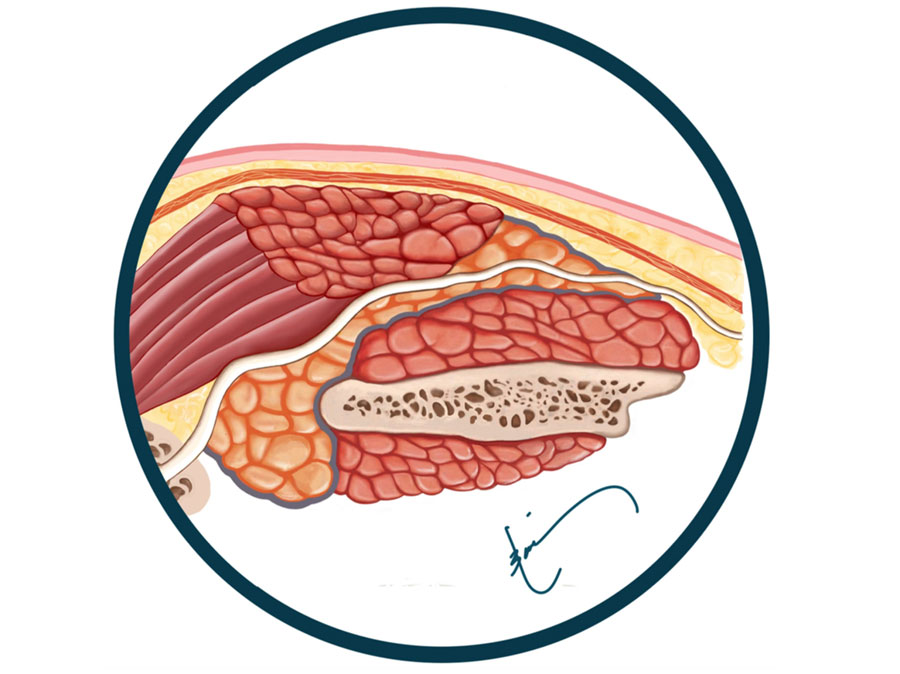
Skin (pink) & SMAS layer (dark orange under
skin) lifted off of parotid. Tumor & a small
portion of additional parotid removed
MICRO-PAROTIDECTOMY FOR A SMALL TUMOR
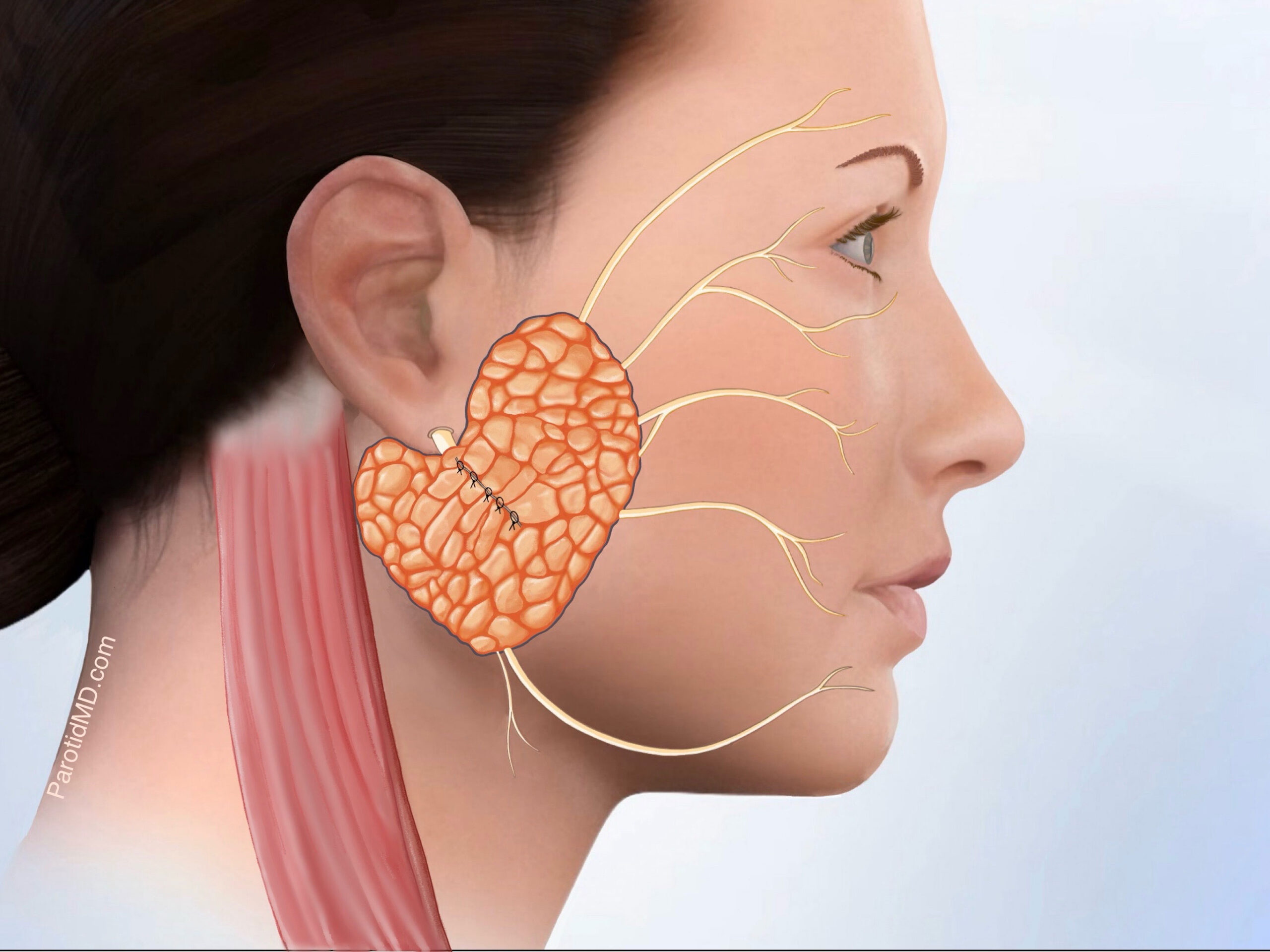
Superficial parotid tissue brought together
& sutured. Facial nerve covered
Parotid tissue sutured together
Facial nerve fully intact & covered

Incision closed with absorbable sutures
under the surface
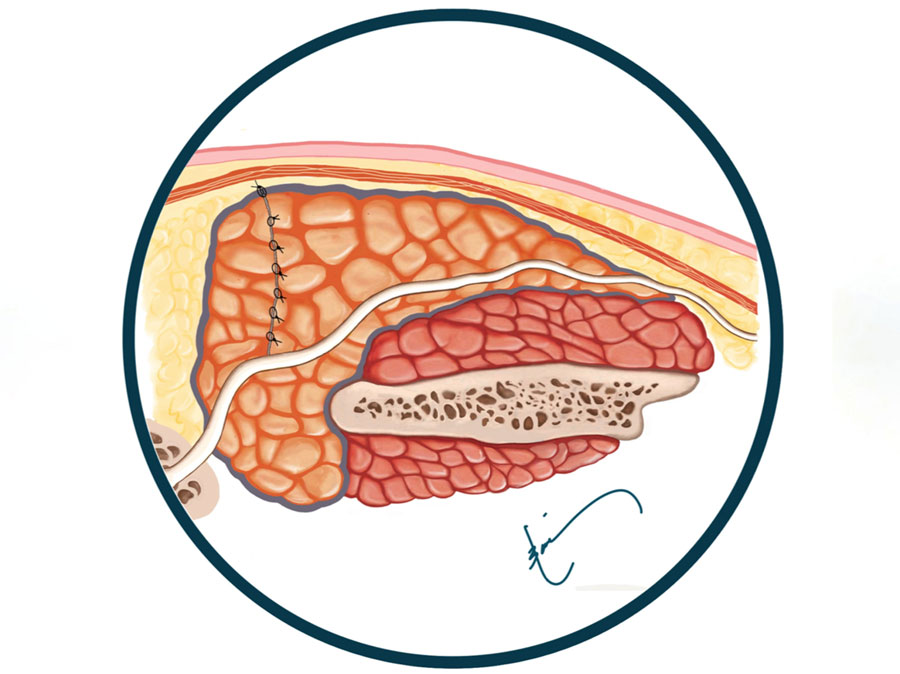
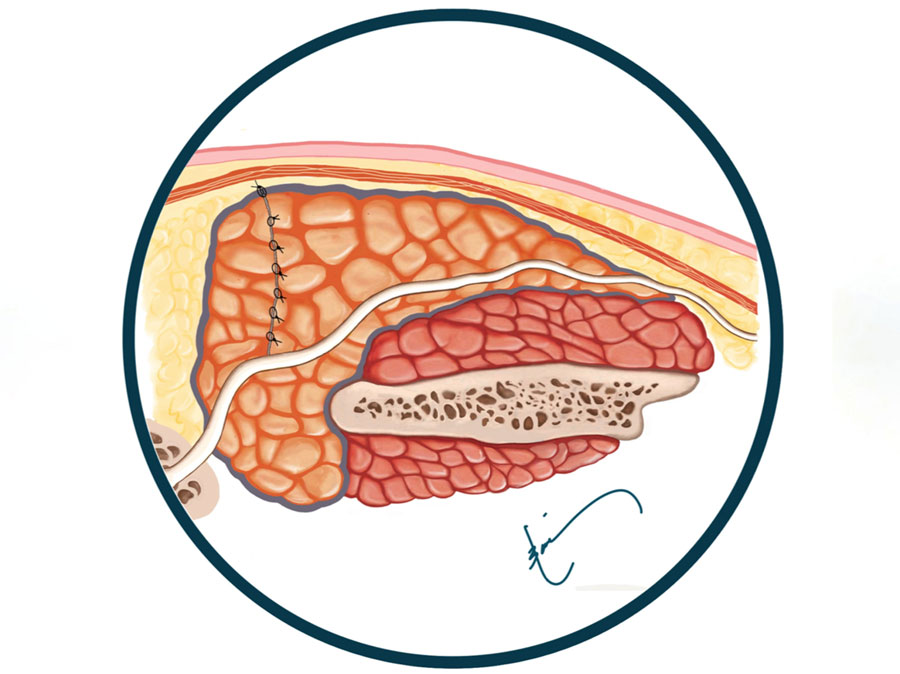
SMAS layer (dark orange) is preserved &
placed between skin & parotid to prevent
Frey’s syndrome, & create smooth contour
MICRO-PAROTIDECTOMY FOR A LARGE TUMOR
Large parotid tumor (grey)
SCM muscles & facial nerve branches
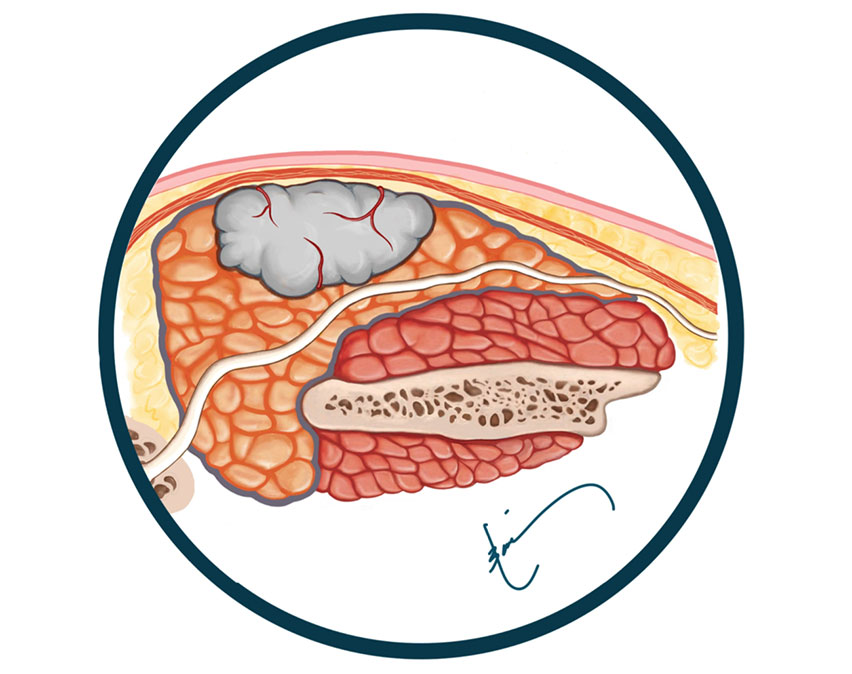
Cross-section of a superficial lobe tumor
Facial nerve (white) going through parotid
Facial nerve & branches identified
protected. Then the tumor is removed
with an extra cuff of normal parotid tissue
Cross-section of parotid & tumor removed
Facial nerve identified, preserved & exposed
MICRO-PAROTIDECTOMY FOR A LARGE TUMOR
A small portion of SCM muscle (10-15%)
brought into parotid defect. Facial nerve
covered.
SCM muscle placed in the parotid defect.
Facial nerve fully intact & covered
SCM flap does NOT cause neck weakness
or stiffness/limitation in movement.

Incision closed with absorbable sutures
under the surface. Small drain place to
prevent fluid accumulation when muscle
lap is used.
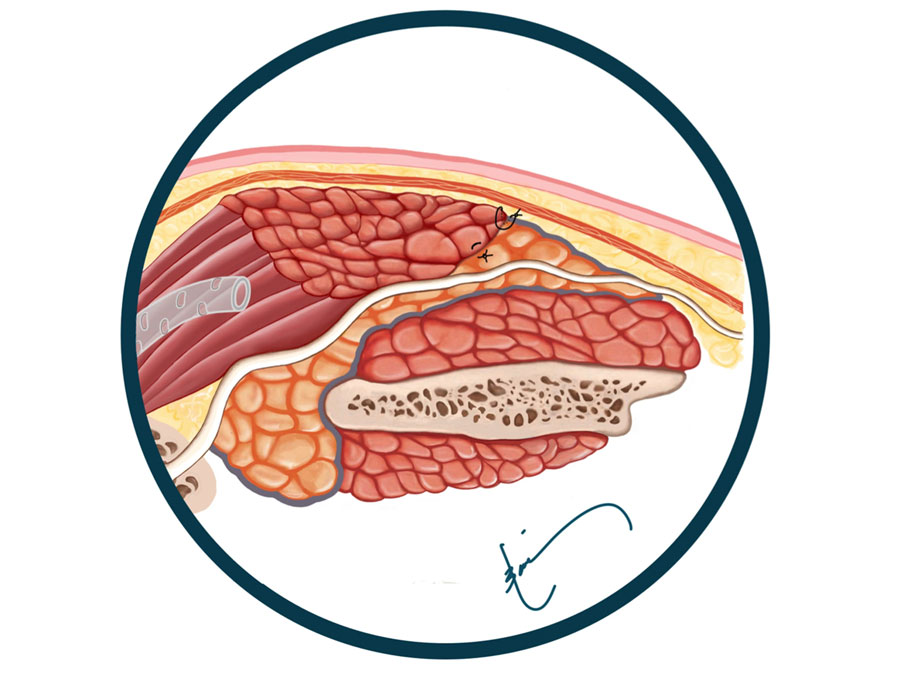
SMAS layer (dark orange) is preserved &
placed between skin (pink) & muscle flap to
prevent Frey’s syndrome & create a smooth
contour. Drain placed next to muscle.
PRESERVATON OF ALL FUNCTION & FACIAL SYMMETRY
Our team of surgeons have unparalleled experience. We take every
safety measure and precaution possible before, during and after surgery to protect and preserve the facial nerve. Therefore, the occurrence of permanent facial paralysis from parotidectomy is extremely low at our CENTER (less than 0.1%). In addition to preserving the facial nerve, we also go to great lengths to protect the greater auricular nerve, which is in charge of providing sensation to the ear lobe. The incidence of Frey’s syndrome is also greatly reduced to significantly less than 1% due to the fact that our team immediately reconstructs the area. THE RECONSTRUCTION ALSO CREATES FACIAL SYMMETRY & HARMONY. When needing surgery on such an important area of the face, it is extremely important to find a surgeon who regularly performs microparotidectomy to protect you from unwanted & avoidable complications.



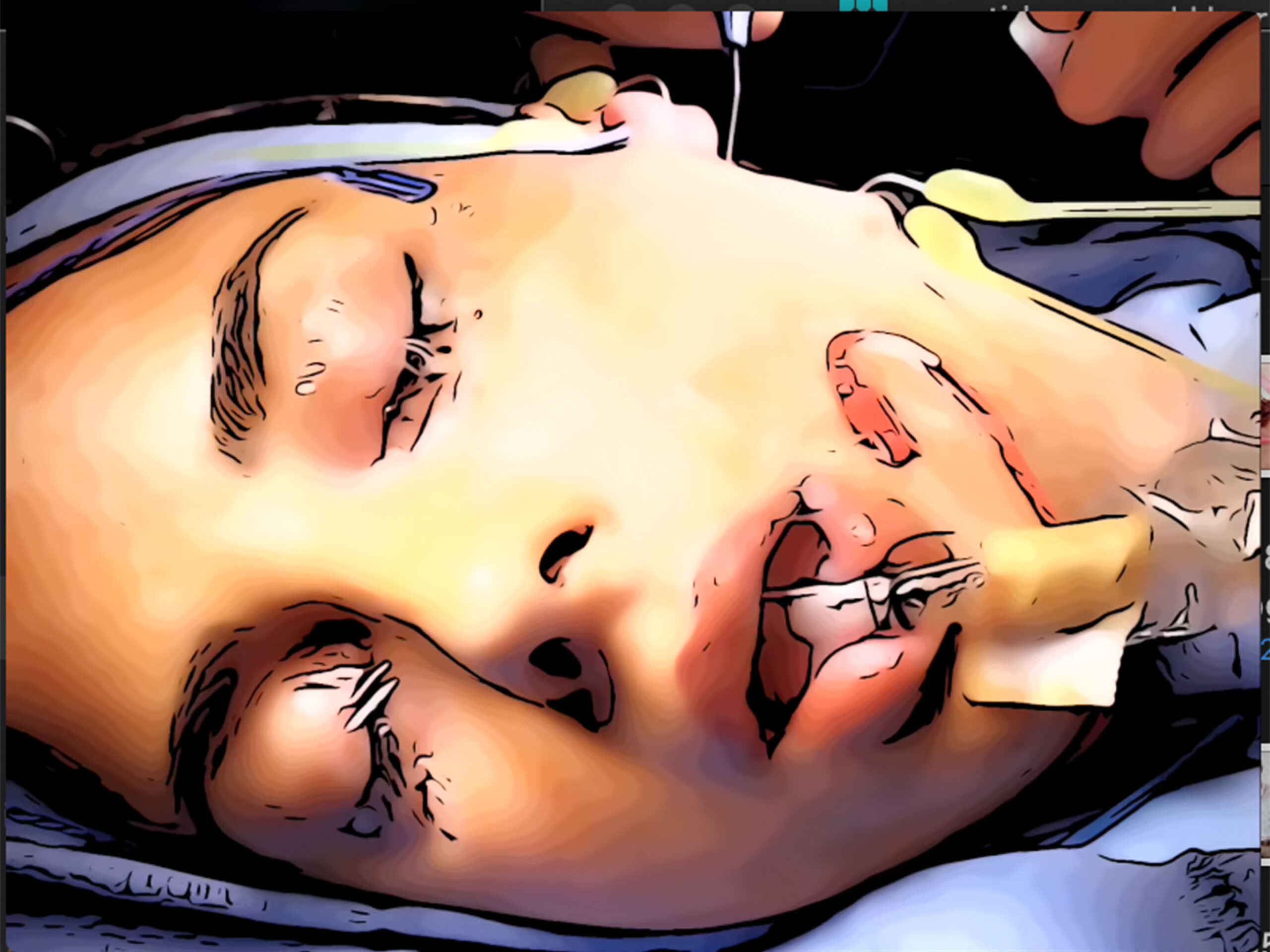
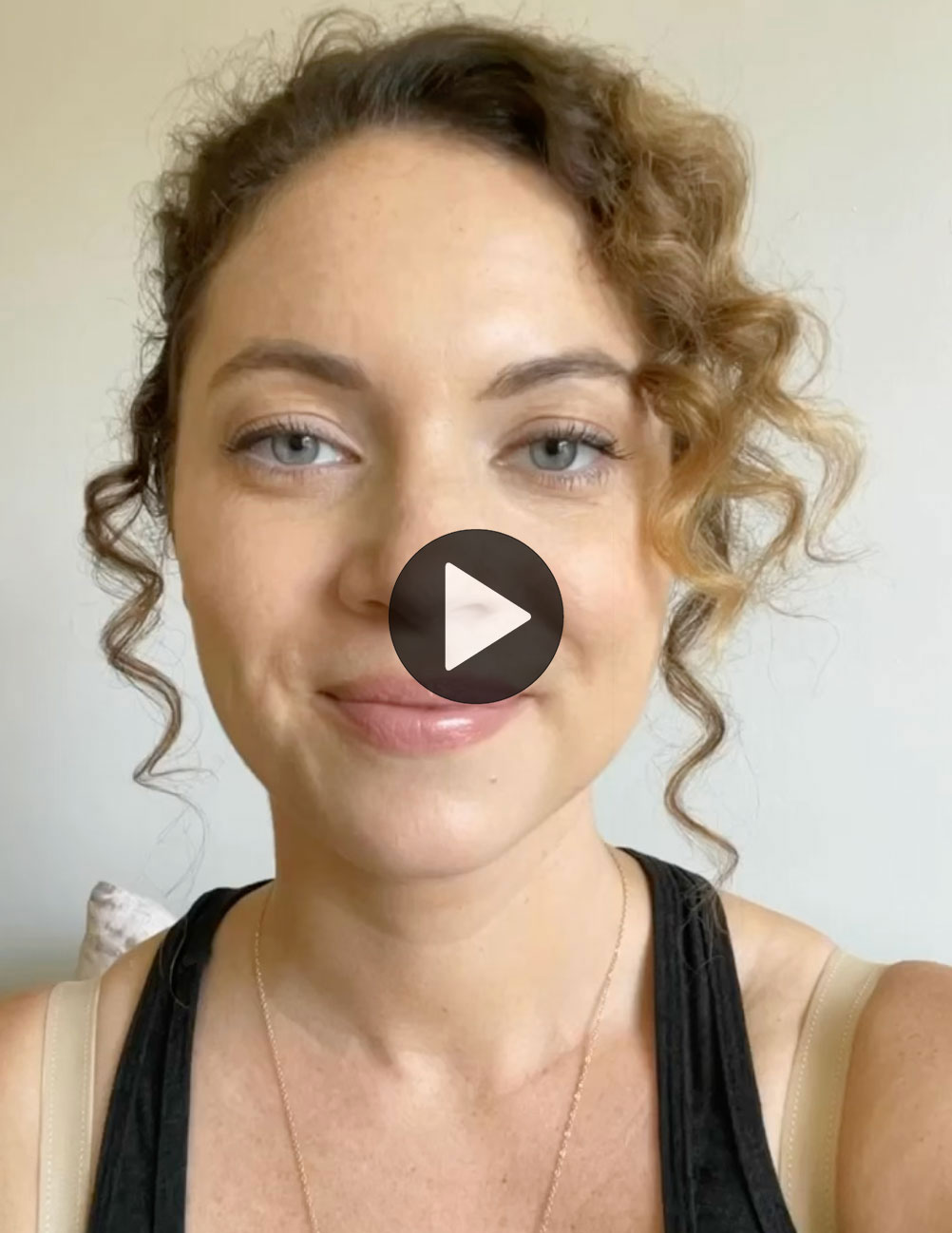
Pictures above the micro-parotidectomy incision at the end of the surgery after it was sutured close in front & behind the ear with dissolvable sutures that are under the surface (do not need to be removed). These are the surgery pictures of the young lady pictured above these set of pictures where the incision is marked in green.
FREQUENTLY ASKED QUESTIONS
What are the reason to treat or do surgery for pleomorphic adenomas?
1. Pleomorphic adenomas continuously grow and become larger.
2. As the grow the start pushing on the facial and in time may entangle the nerve.
3. The potential to transform into an aggressive cancer is considerable, especially if you have a long life ahead.
4. As the tumor grows it forms more fingers (pseudopods) & stretches out the capsule thus increasing the chance of rupture & spillage during surgery



The tumors can present at any size, but unfortunately the great majority invariably grow to become massive if left alone.
Is it possible to not treat or do surgery for pleomorphic adenomas?
This is a very good & difficult question to answer. It is obviously always the choice of the person who has a pleomorphic adenoma to have surgery or not. If there is a compounding factor such as other illness that precludes the person from having surgery or anesthesia (for example heart disease or severe lung disease), then the tumor can be observed closely. This doesn’t stop the tumor from growing or transforming into a cancer, but at least we may catch the tumor that has transformed into cancer earlier in the process.
Over the years I have had a number of patients that were very much fearful of surgery and were being monitored with repeated exams and scans. The great majority of them ultimately have had surgery. And the reasons to proceed with surgery for them were: (1) tumor growing to be large and very visible (2) sudden growth and the fear that it has turned into cancer (3) overwhelming anxiety of having a tumor in their body. All of them very happy that they had surgery, mostly because micro-parotidectomy has a very low level of pain or discomfort, it was outpatient (not requiring hospitalization), their facial nerve was fully functioning, the recovery was very rapid, and they had no complications.
Are there any patients that Dr. Larian recommends not to have surgery?
Yes, older patients that are frail or have other illnesses that potentially shorten their lifespan. And in these cases, when the person lives in another city, state or country I can coordinate monitoring with their local doctor.
Is the greater auricular nerve cut during microparotidectomy?
Denitely not. The greater auricular nerve (GAN) is immediately under the skin & during every parotid surgery it is preserved. It is in charge of feeling of the earlobe and the skin around the lower part of the ear and over the parotid. It may be at times in our path to get to the other important nerve (facial nerve) in which case the nerve is identified, separated from the parotid and preserved out of the way.
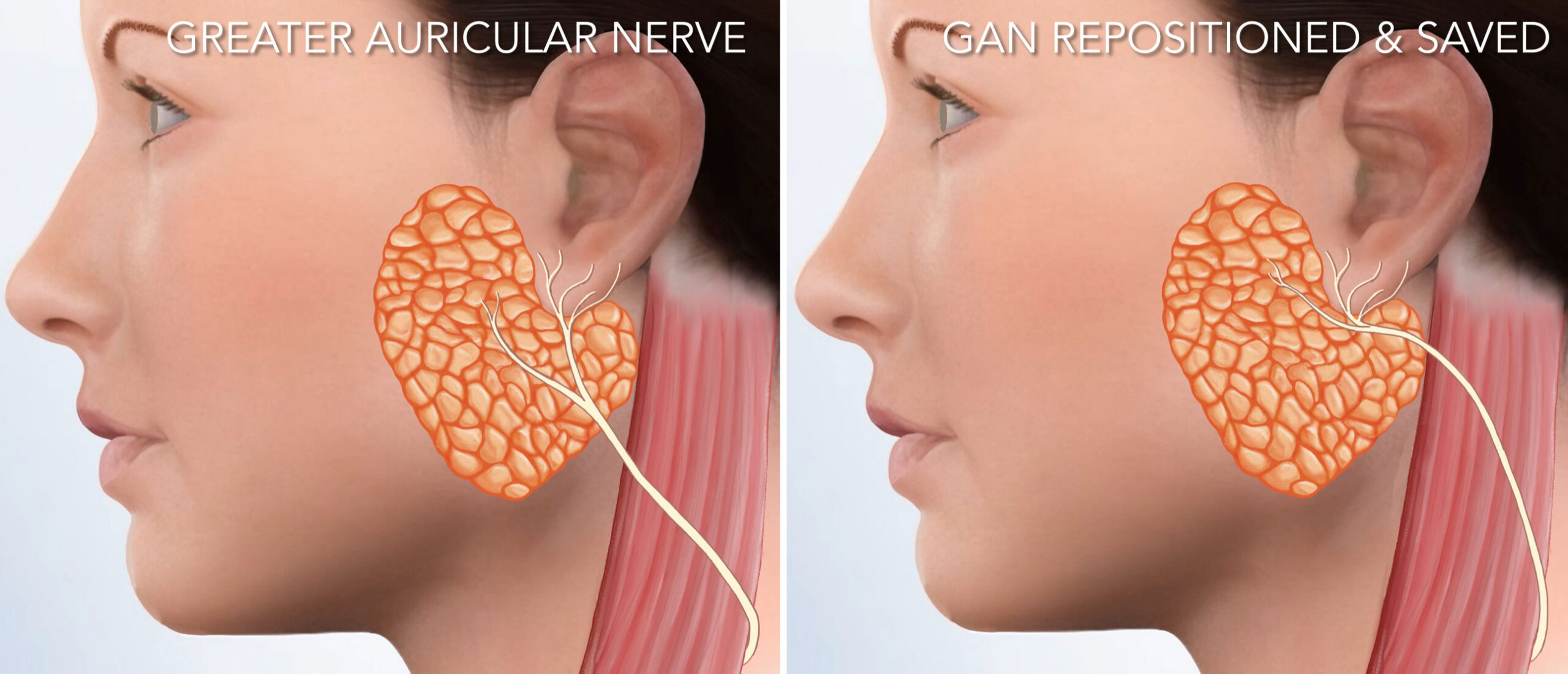
This may make the GAN temporarily not work well, which can cause numbness in the area of surgery (parotid). Which is in fact a big advantage because numbness in the area after surgery makes this a relatively pain free surgery. Fortunately the numbness is short-lived, and the feeling in this area returns usually within 6 weeks.
Are any of the branches of the facial nerve cut during micro-parotidectomy?
Absolutely not. The facial nerve is too important for any of its branches to be compromised. Majority of the time during this surgery is spent on identification of the facial nerve and its branches. Facial nerve expertise is of vital importance as is attention to detail and patience. There is no reason to not take extra time to try to preserve every single branch of this vital nerve.
Are the facial nerves monitored during micro-parotidectomy?
Yes, in every single case a facial nerve monitoring system is used.
This system continuously checks the activity of the facial nerve. When it senses the slightest activity close to the nerve it sends alerts. The alarms let the surgeon know they are close to the nerve and to exercise extreme caution. This is no substitute for expertise but is an additional measure of safety for the nerve. In the video the monitors can be seen as blue probe, next to the eye & red probe for the lip.
What other measures are taken to assure the integrity of the facial nerve during micro-parotidectomy?
After all the facial nerve branches in the area of the surgery are
identied and then the tumor removed; then each of the branches of
the facial nerve are stimulated with a Checkpoint nerve stimulator to
make sure each branch is working to definitively confirm during surgery that the facial nerves are intact and functioning.
Can large deep lobe pleomorphic adenomas be removed through the micro-parotidectomy approach?
Yes. In fact, it’s the preferred method at the CENTER. In the MRI images to the right you see a large tumor (bright white) starting from the parotid and pushing into the throat. However, on MRI the tumor appears to be in the area where the facial nerve enters and courses through the parotid. As such, it is imperative that the tumor be removed after the facial nerve and the branches are identified to assure they remain safe. In the animated video of the live surgery below you can see the large tumor seen on MRI being brought out through the micro-parotidectomy approach. This is followed by reconstruction of the area.
Micro-Parodectomy for a deep lobe tumor extending into the parapharyngeal space. The actual surgery has been transformed into animation. The whole tumor is gently and meticulously separated from the surrounding tissue & removed.
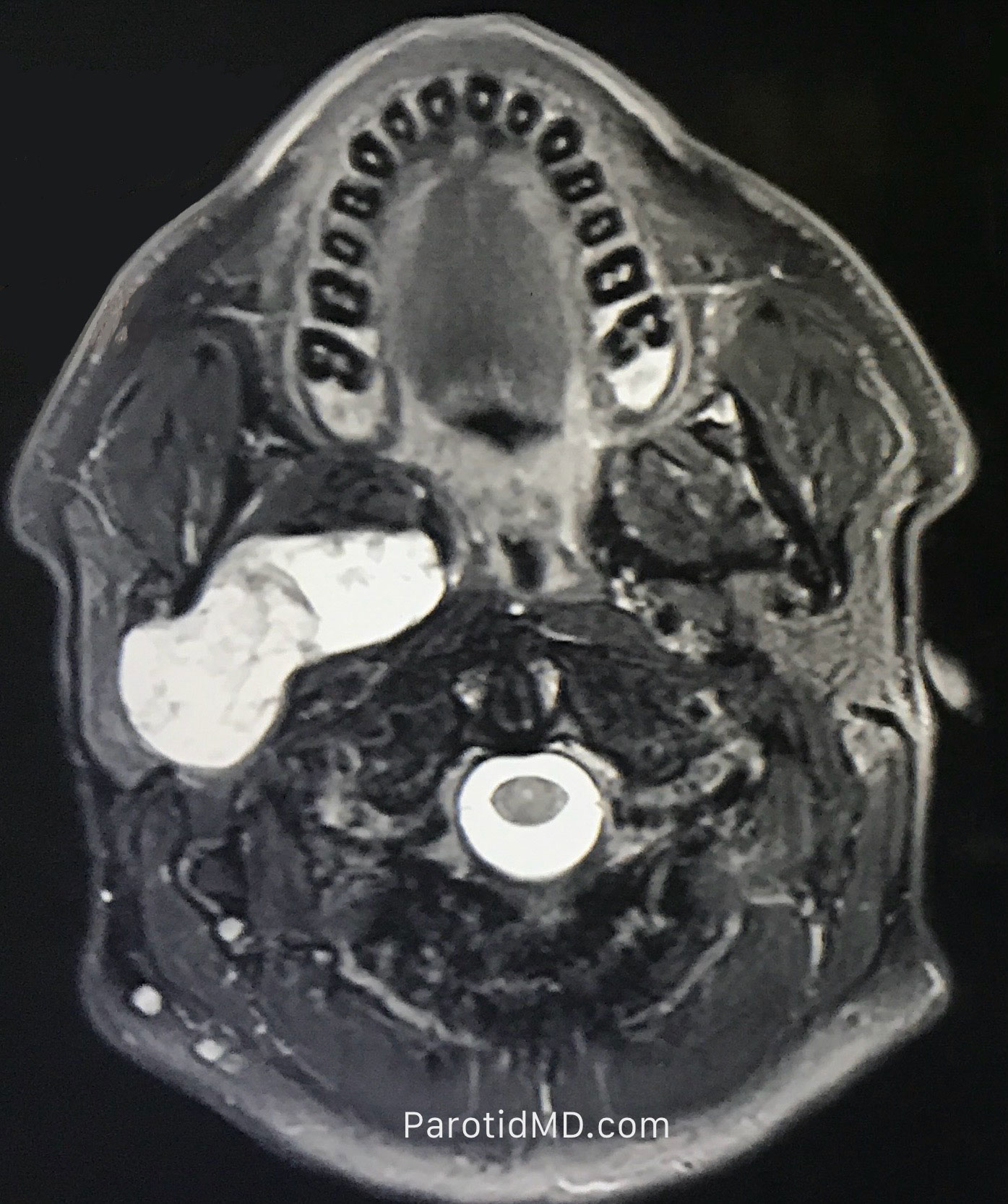
MRI - Pleomorphic Adenoma extending from the deep lobe into the parapharyngeal space (next to the throat).

Meet The Team
Led by board-certified parotid surgeon, Dr. Babak Larian, our team of specialists has decades of experience successfully diagnosing and treating diseases of the parotid glands with minimally invasive procedures. Distinguished by our compassionate care and cutting-edge techniques, the CENTER has developed a reputation for delivering the best parotid tumor surgery available.