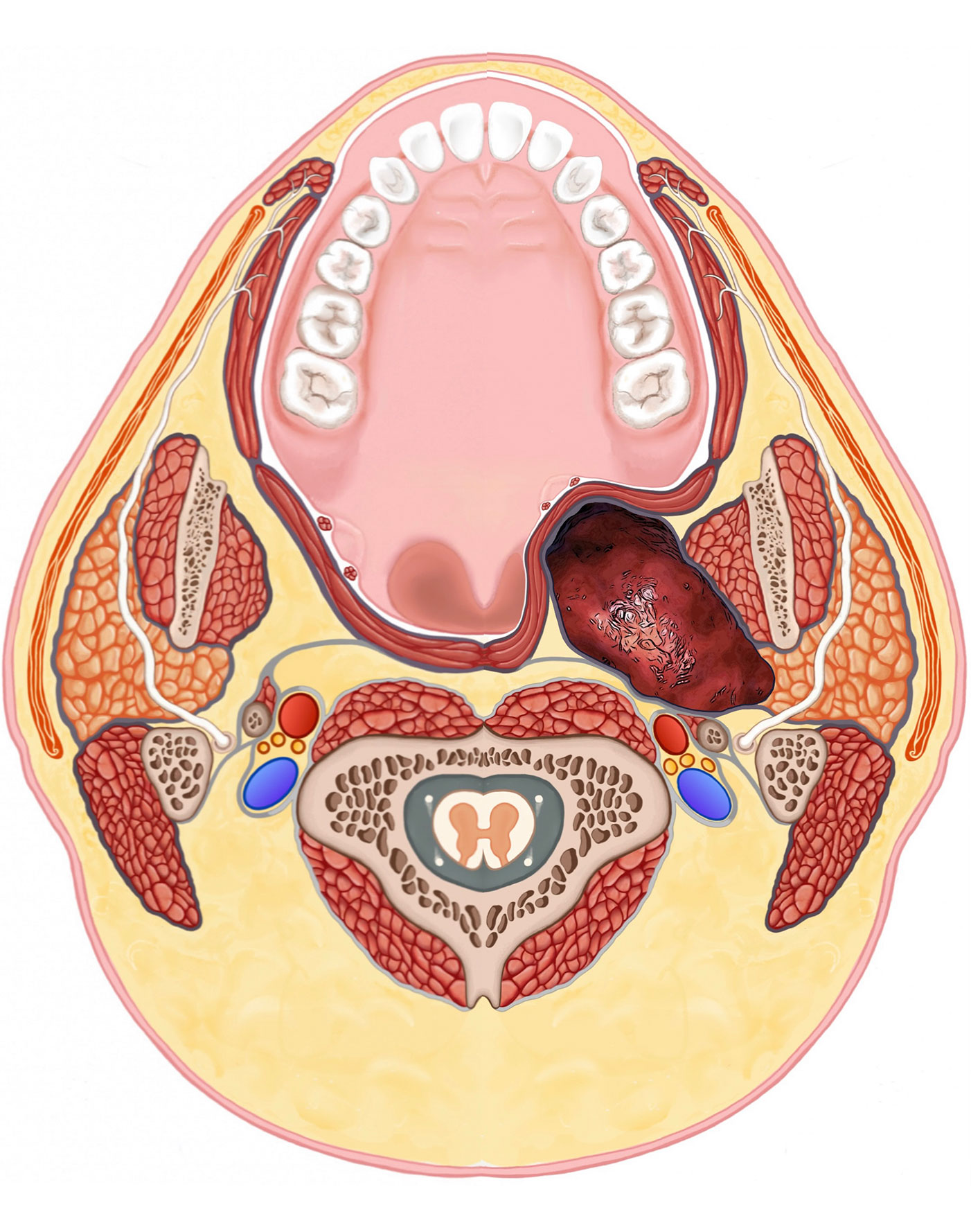
The area of parotid deep to the facial nerve is considered the deep lobe. Further deeper is a rectangular shaped space that sits deep to the jawbone & muscle, just behind the throat called the parapharyngeal space. It is called parapaharynx because it sits next (para) to the throat (pharynx). There are a lot of important structures in this area.
PARAPHARYNGEAL
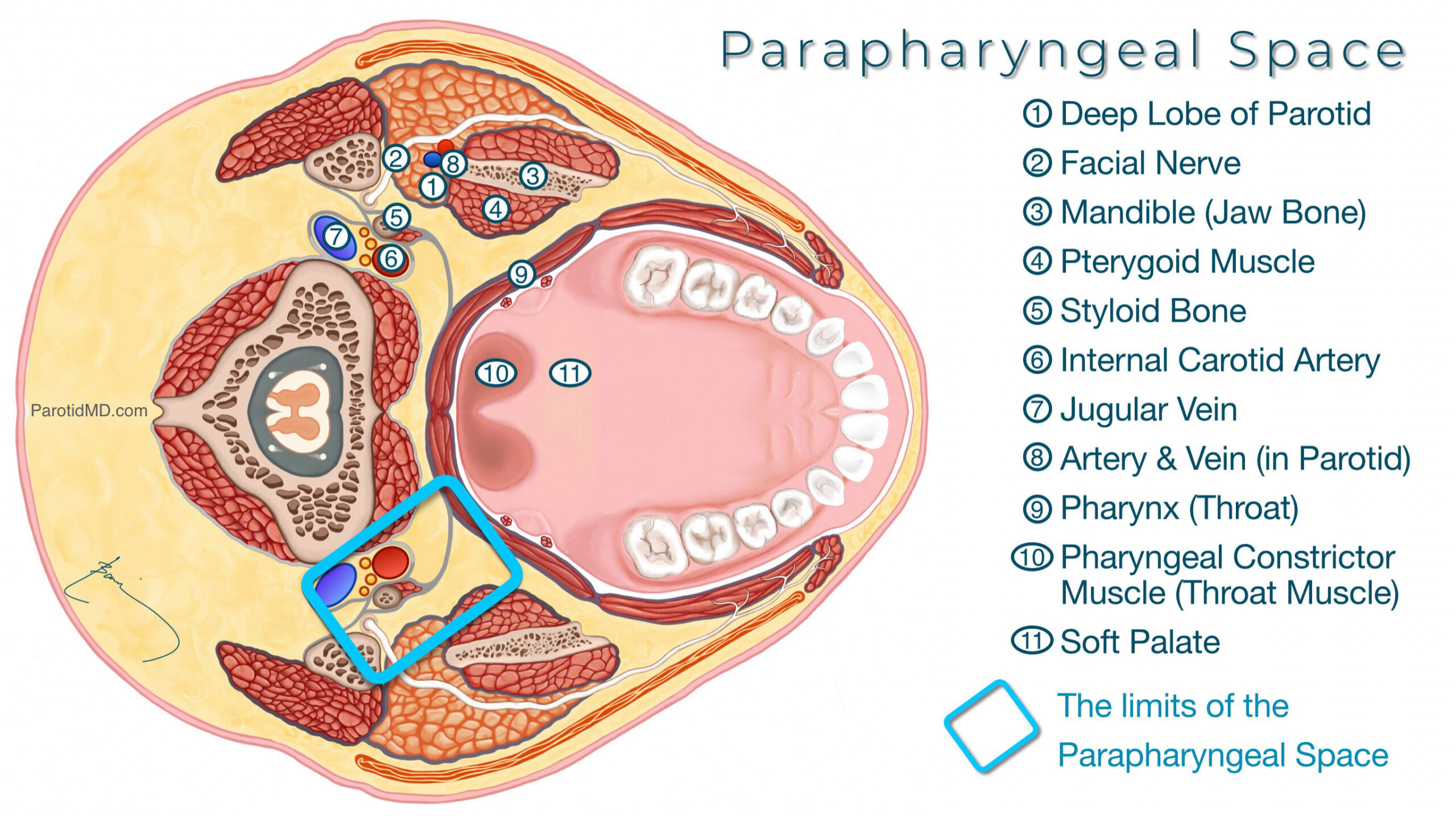
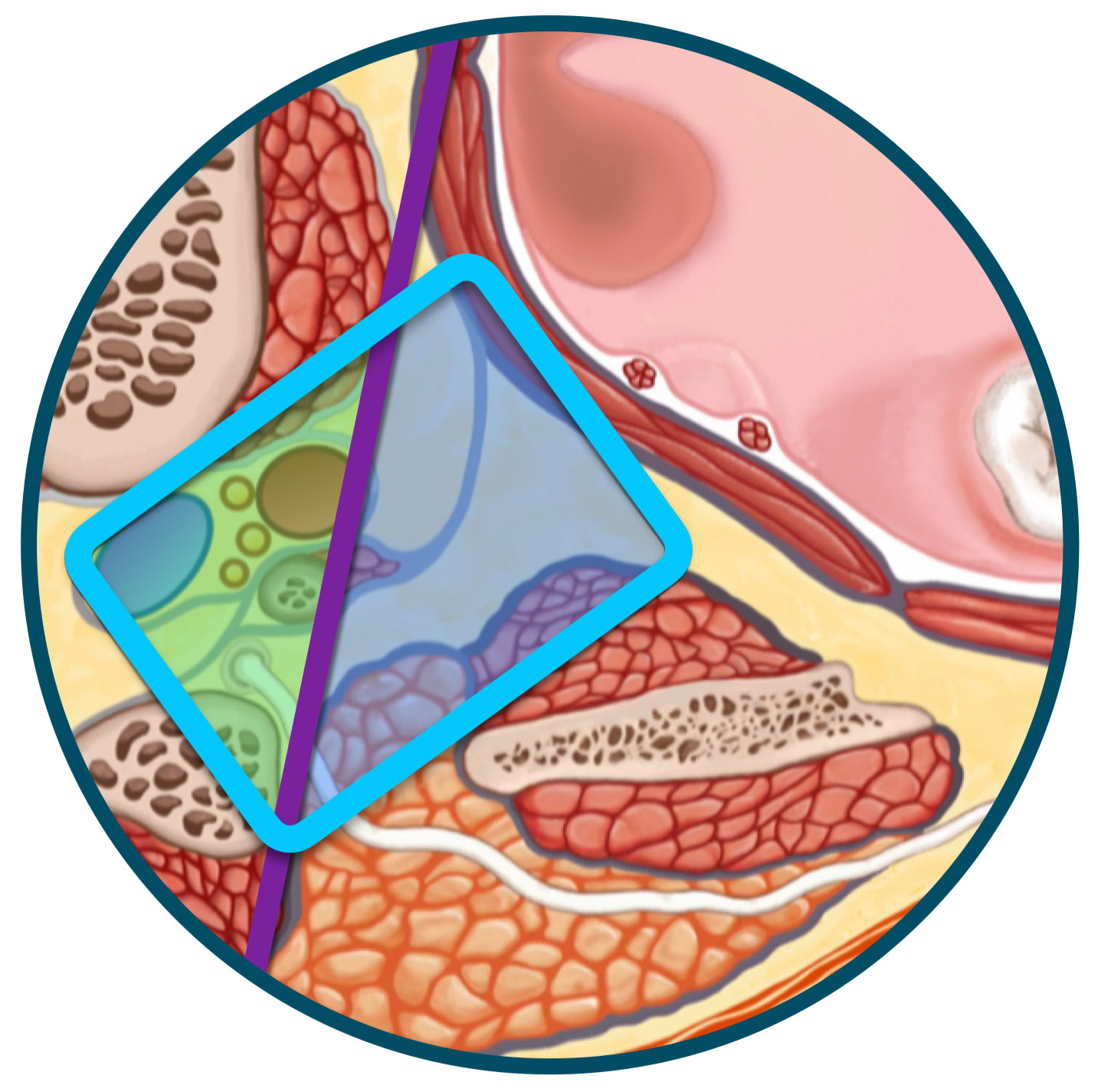
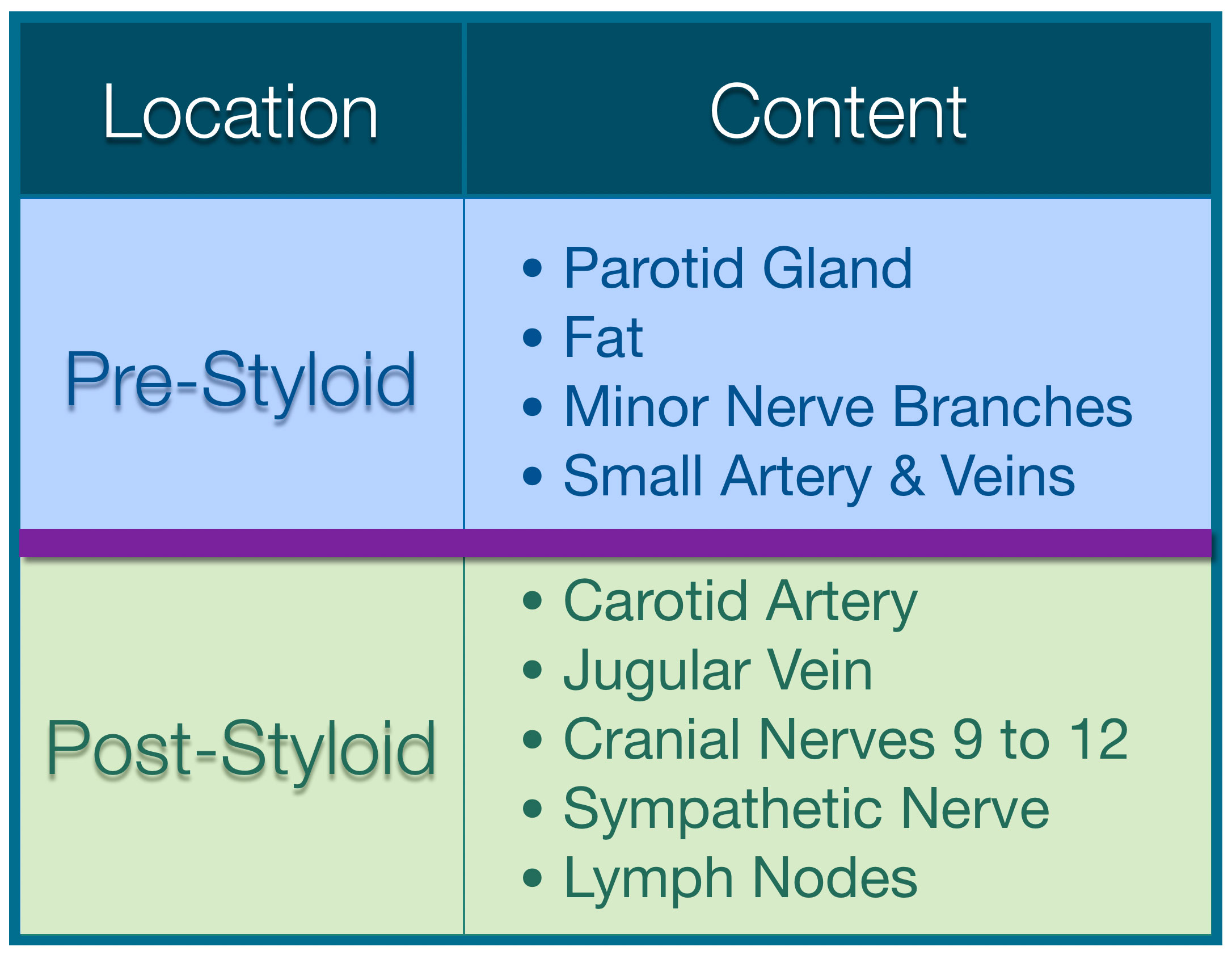
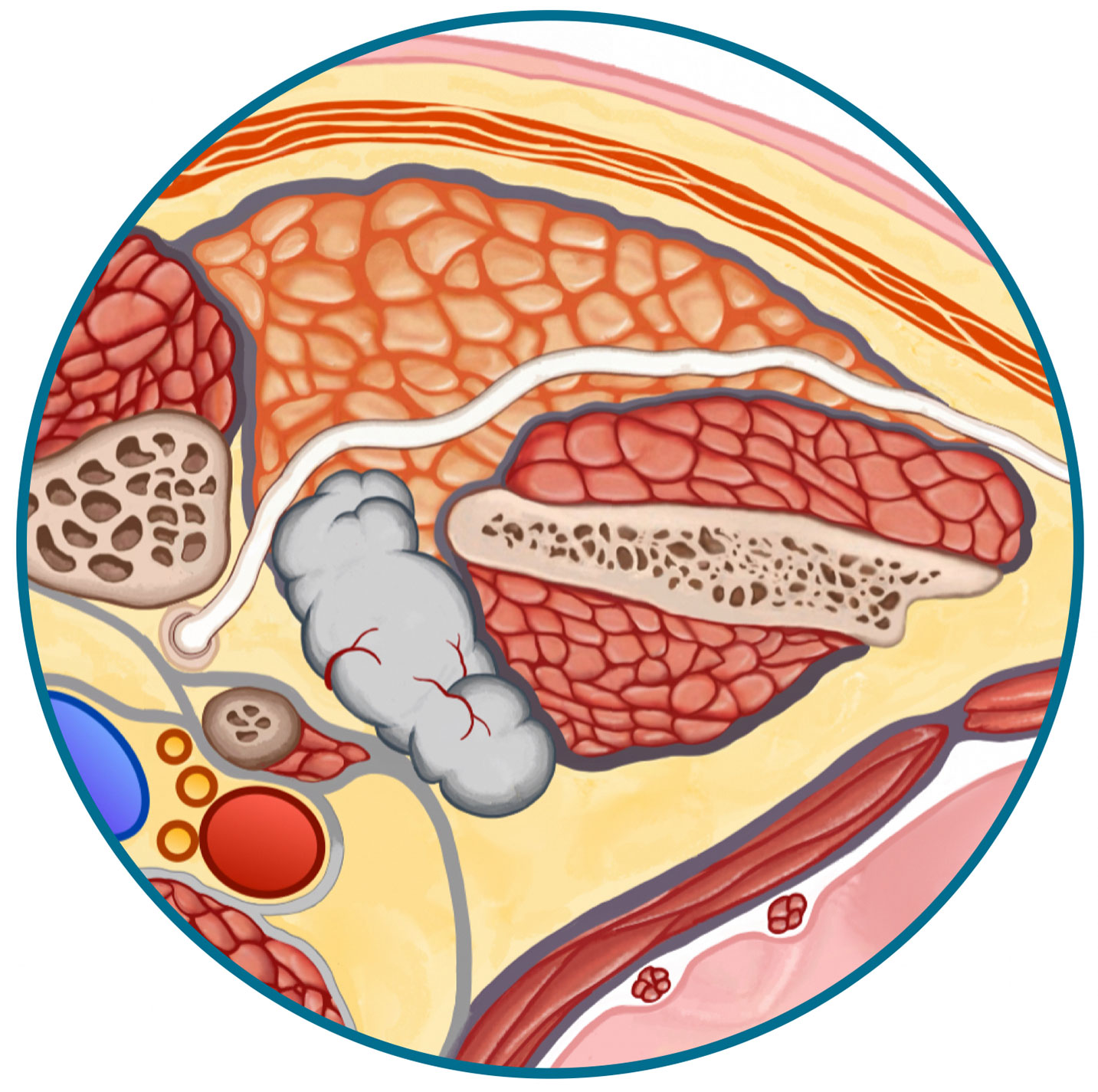
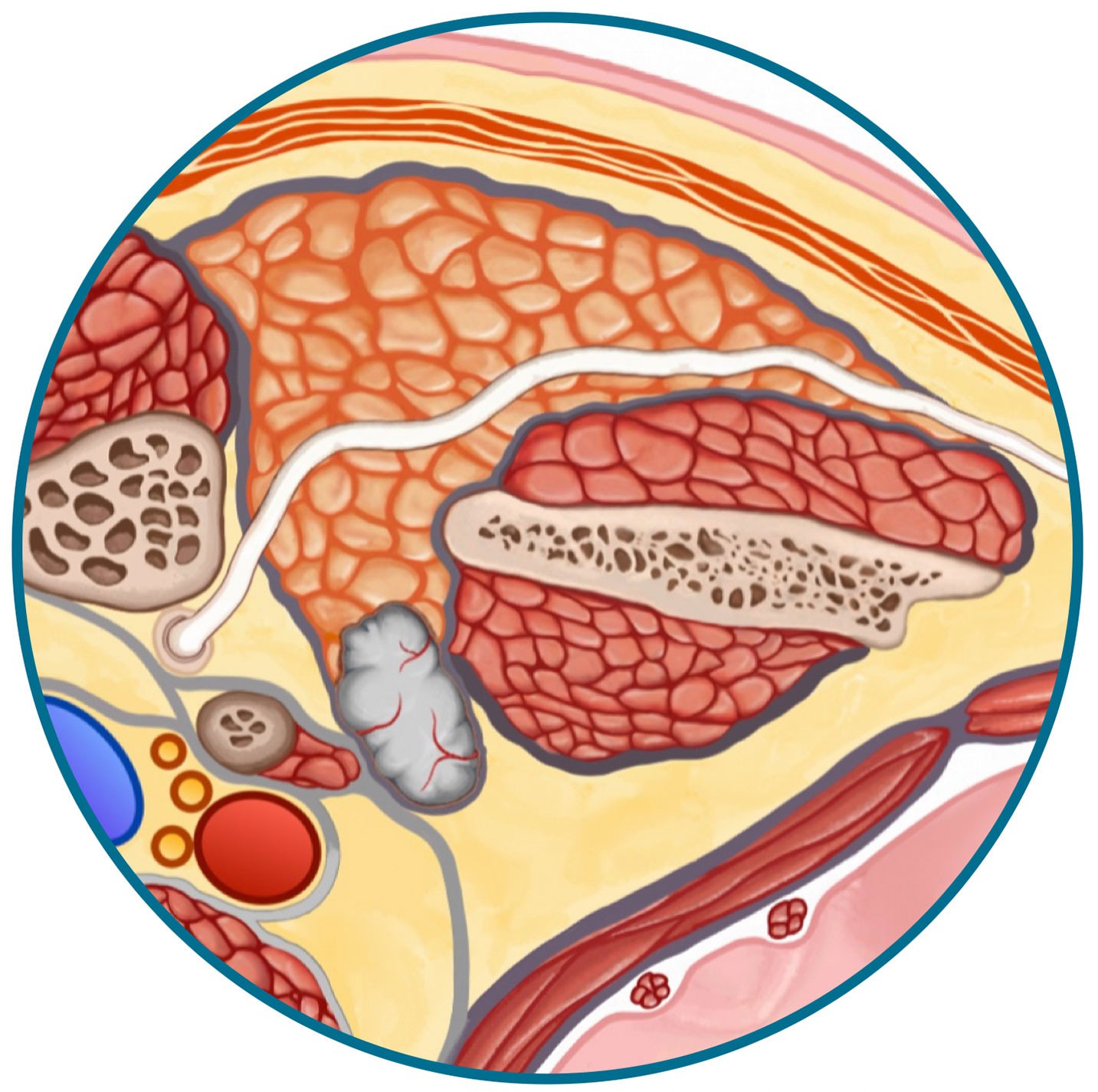
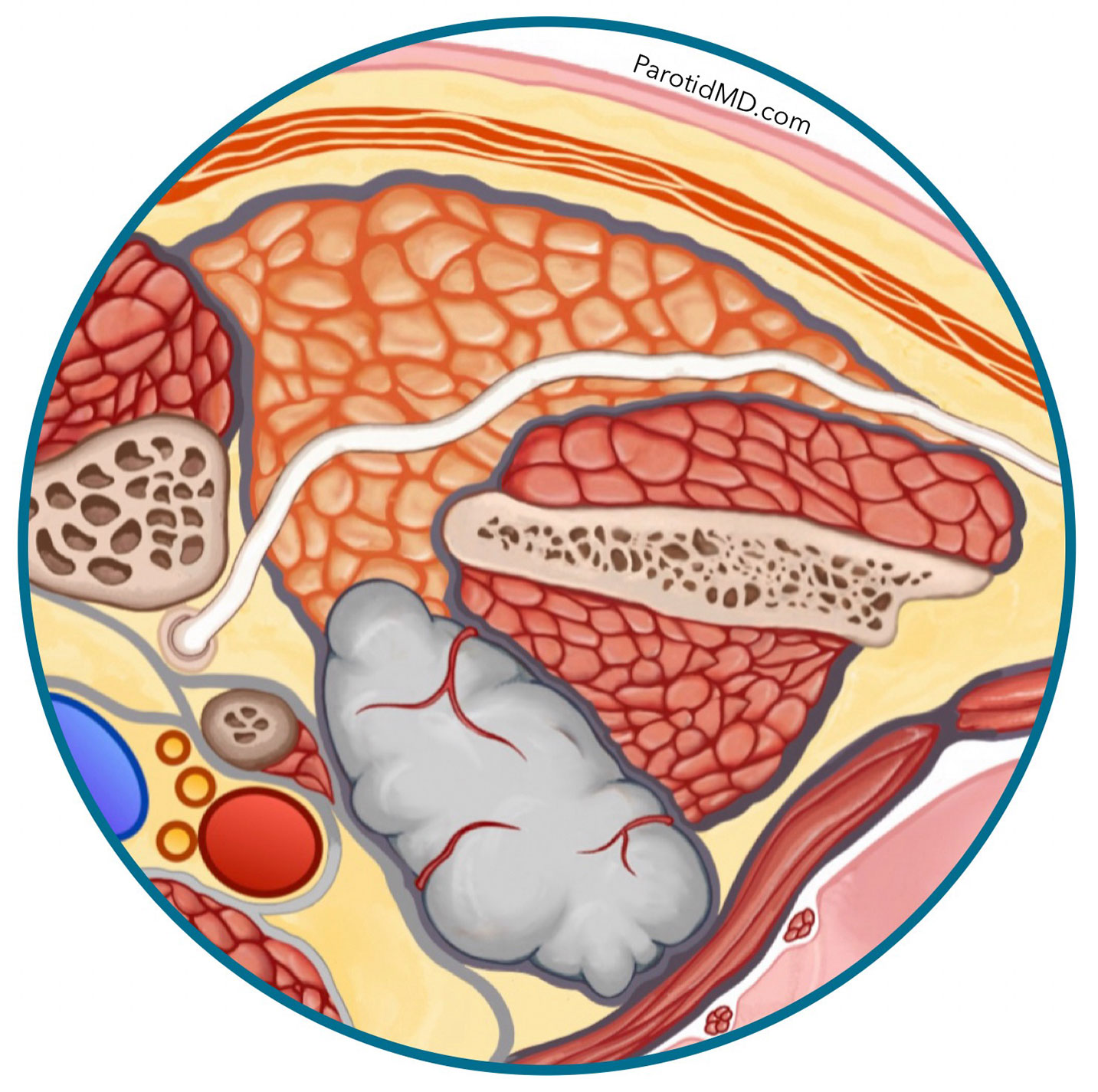
The parapharyngeal space is divided into two compartments by the STYLOID BONE. The area in front of the Styloid Bone is called the pre-styloid space & the area behind it is called the post-styloid space. The post-styloid space contains very important structures: blood vessels and nerves. While the pre-styloid space leads from the deep lobe of the parotid into a space that is mostly filled with fat (yellow) and heads towards the throat (pharynx).
In the magnified image below the Blue Square shows the outline of the parapharyngeal space. The purple line separates the prestyloid space (blue shaded area in the blue square) & post-styloid space (green shaded area). The content of each compartment is listed in the table below.
Parotid tumors that grow into the parapharyngeal space tend to be constrained by the skull bones, jawbone & jaw muscle, and Styloid bone & muscles, which forces the tumor to grow in a forward direction towards the throat. The pre-styloid space is a much safer space to do surgery in as it contains a lot less structures & very little risk (in the hands of an expert surgeon).
2 Growth Patterns
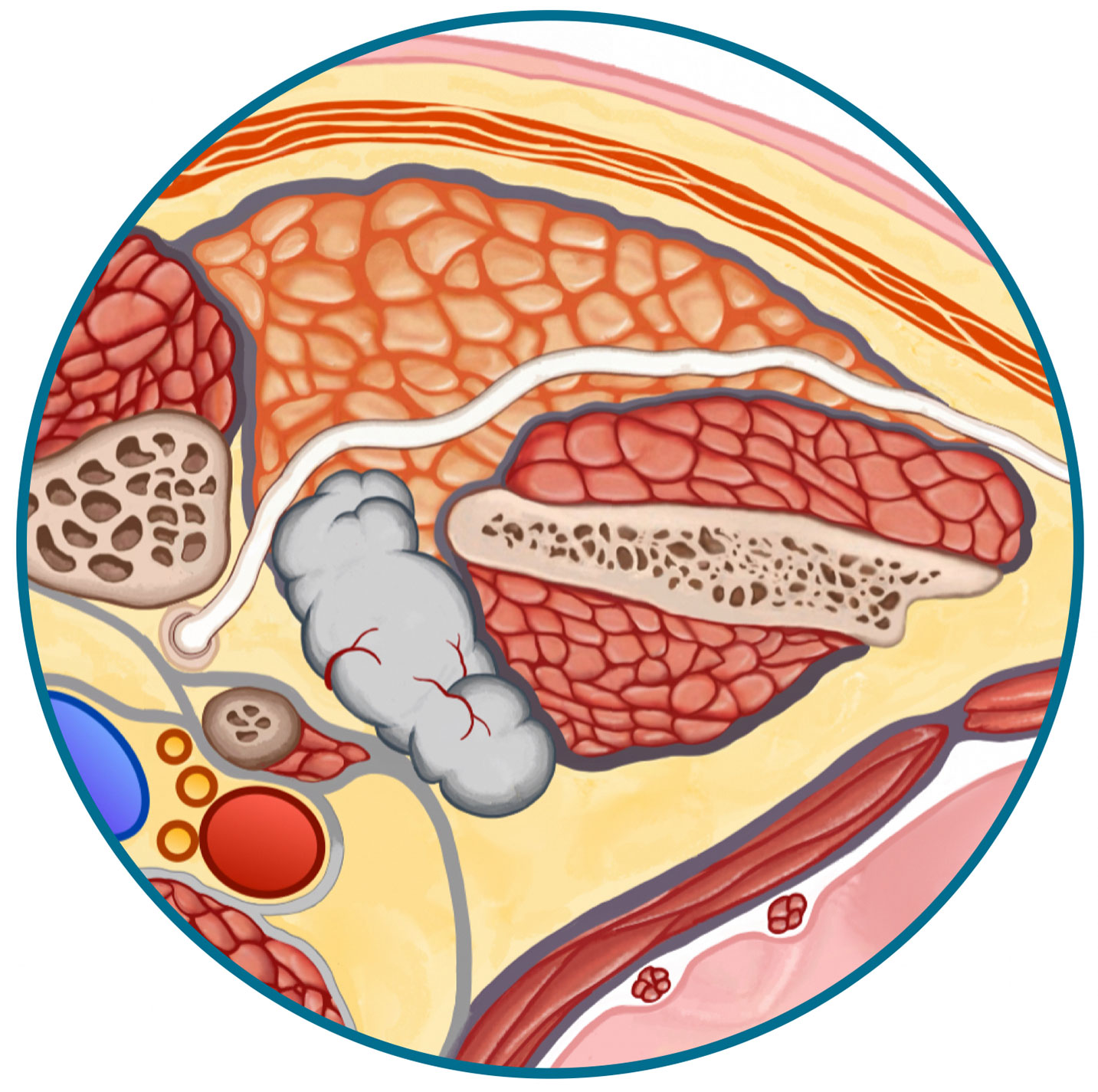
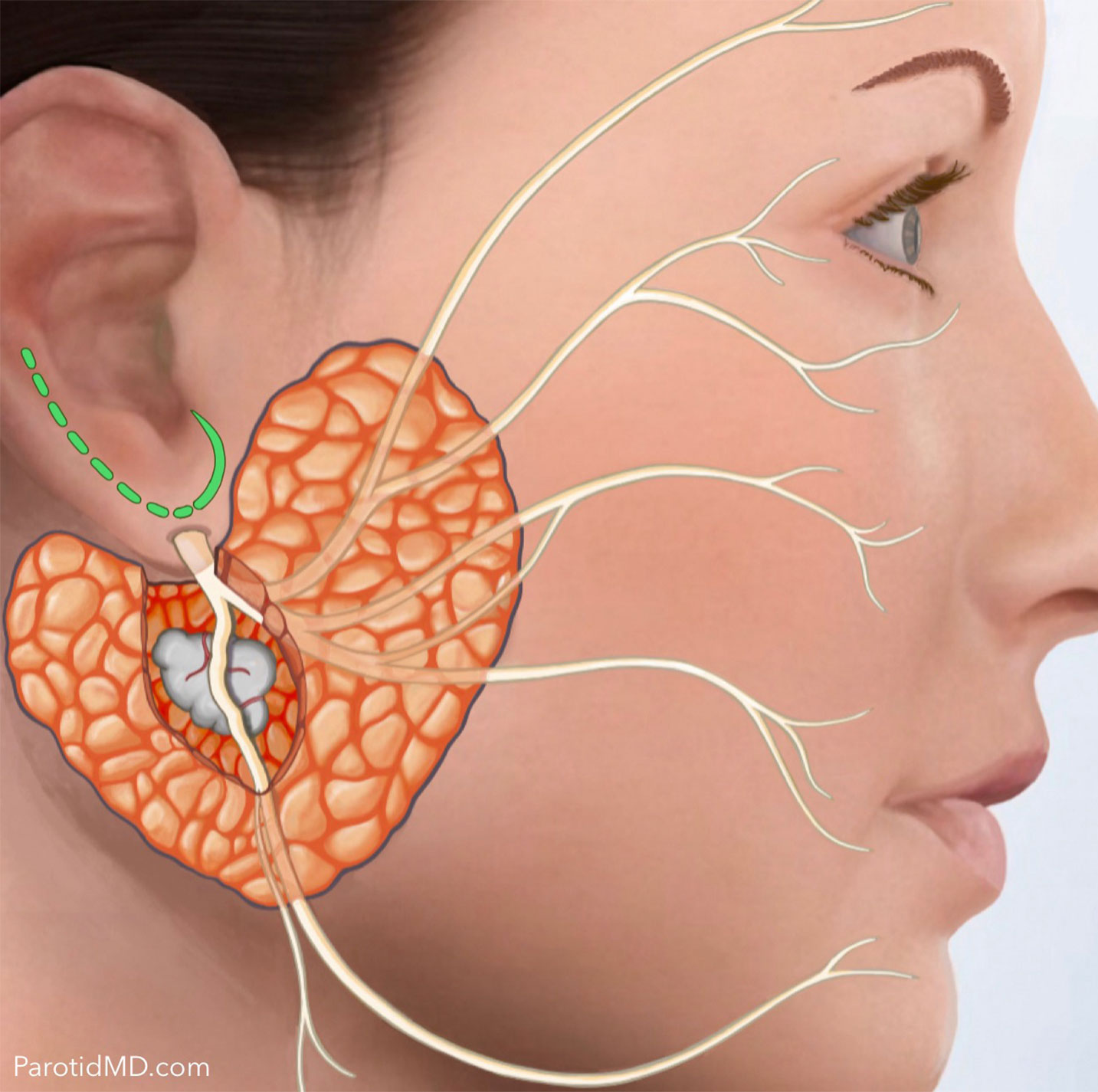
Tumors that start in the deep lobe closer to the facial nerve, can grow into the parapharyngeal space. These tumors are most often in close contact with the facial nerve.
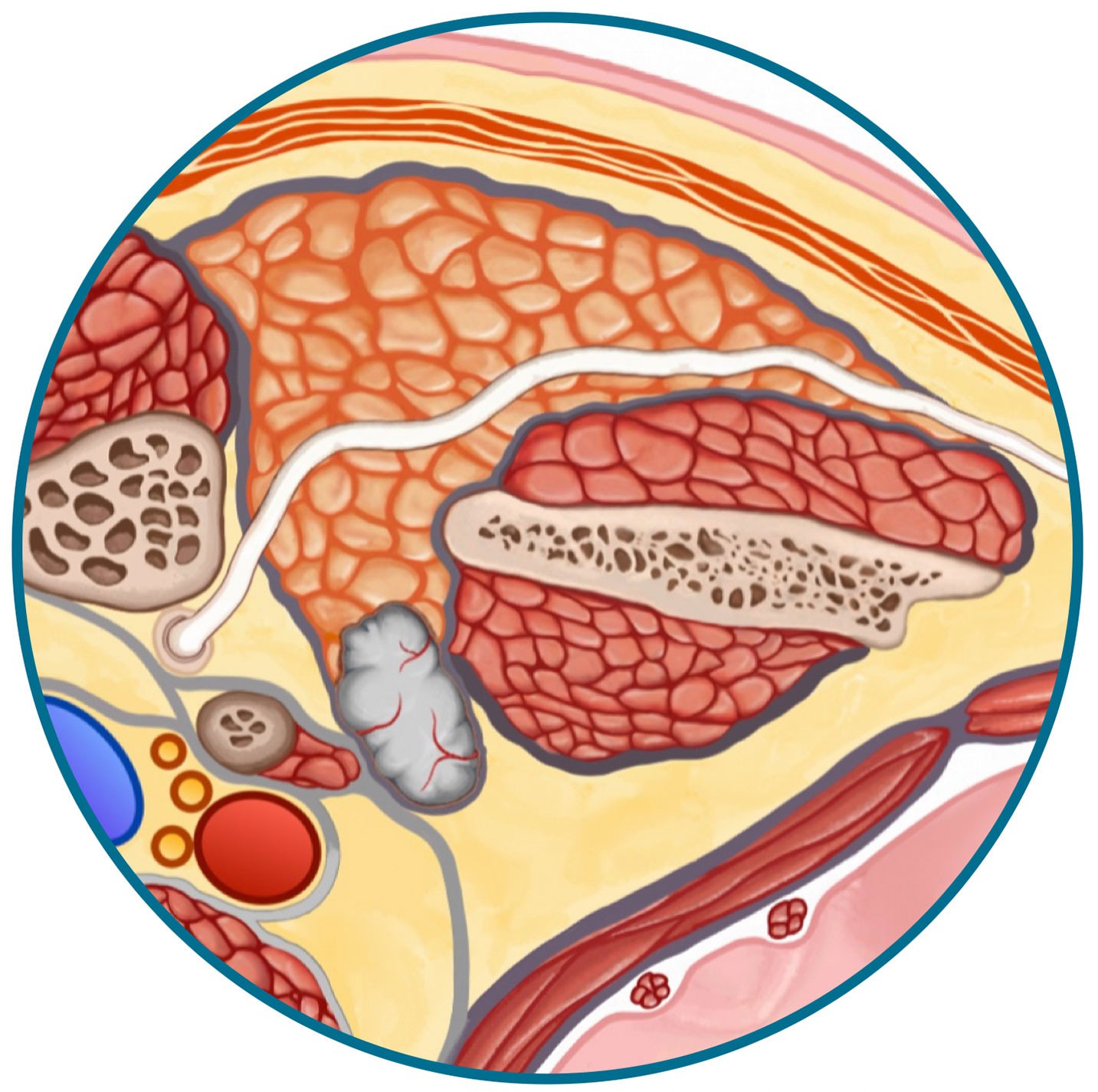
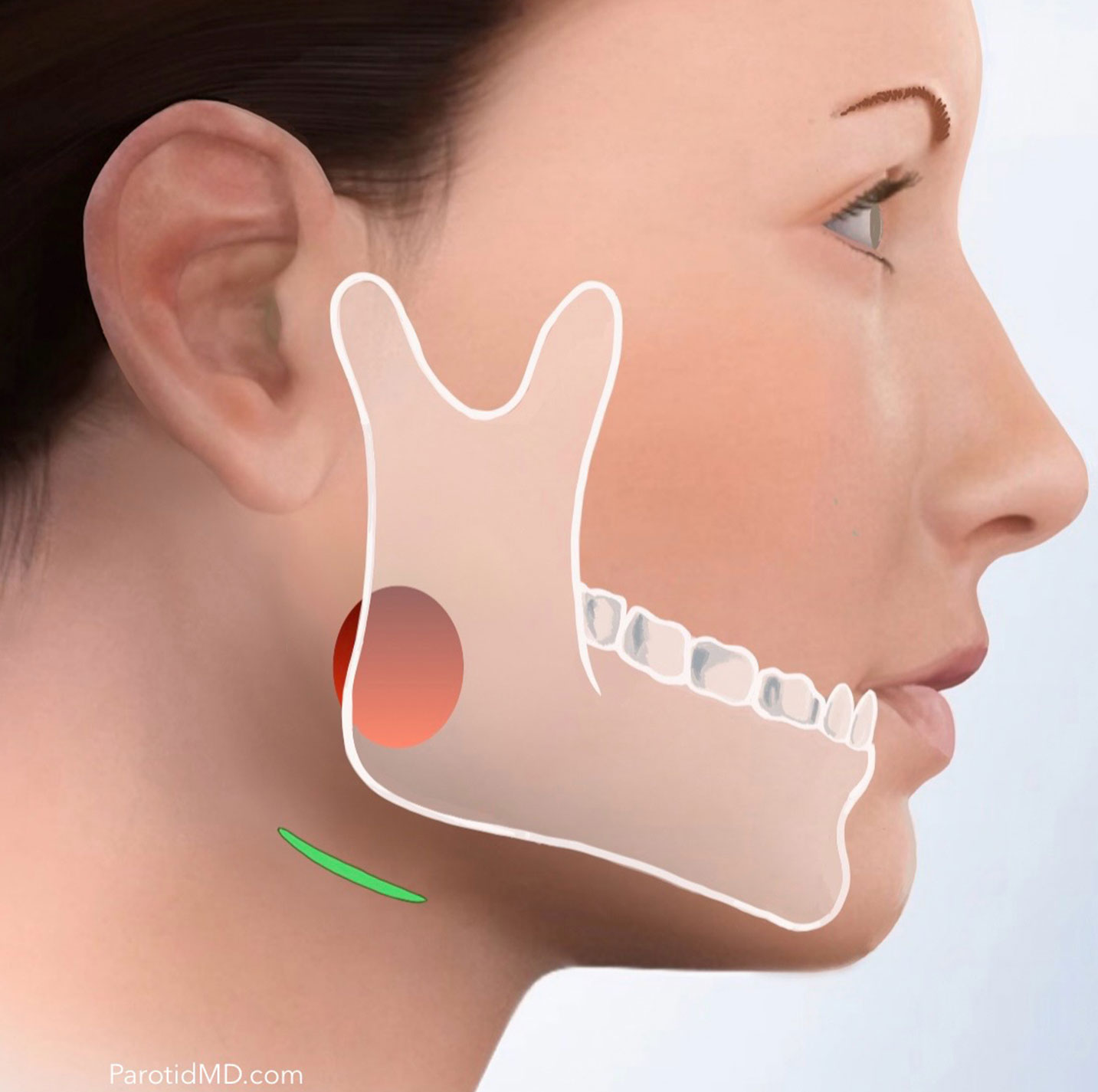
Tumors that start at the tip of the deep lobe can grow into the parapharyngeal space. These tumors are generally a safe distance away from the facial nerve.
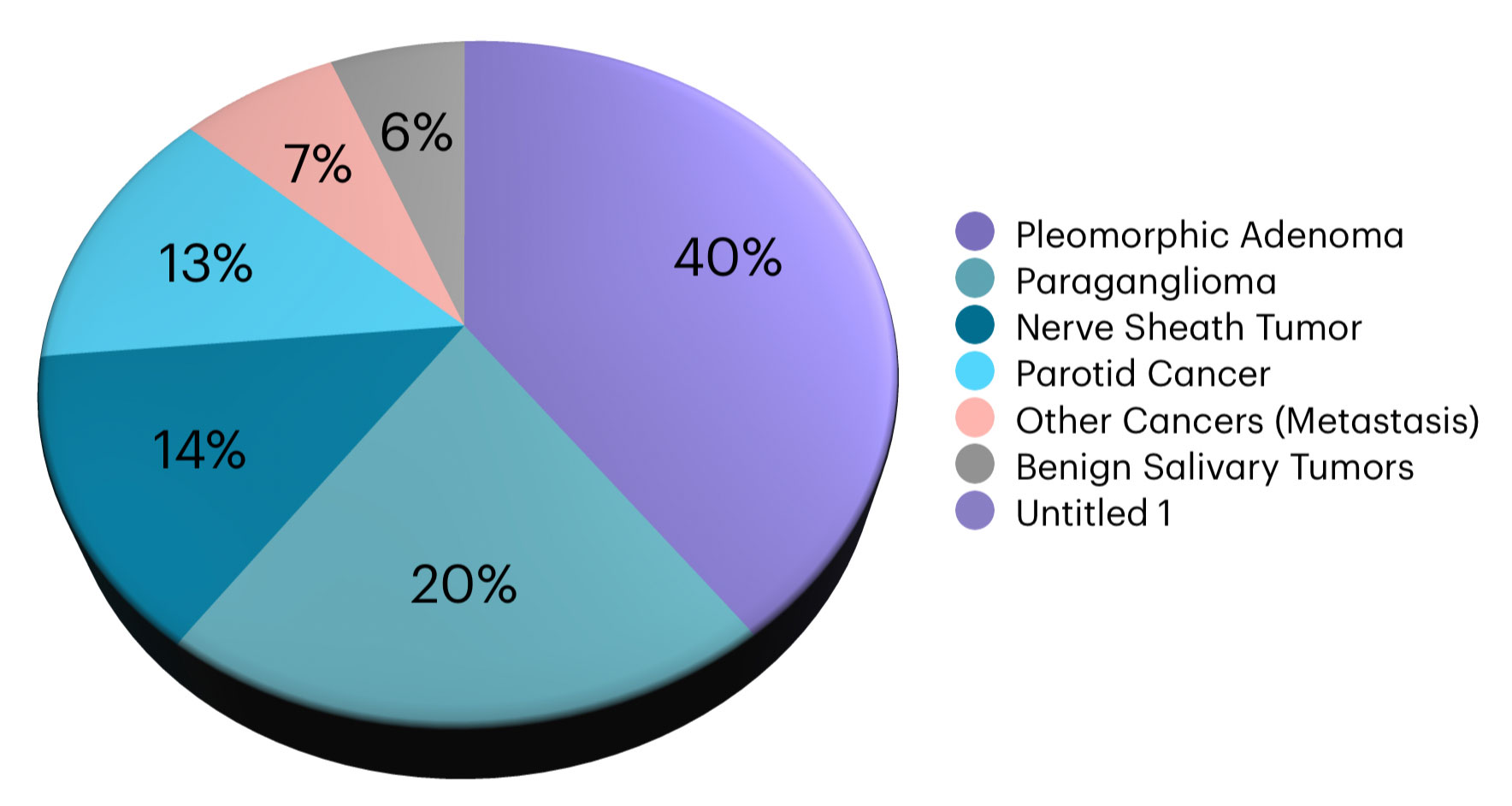
Types of Tumors
The types of tumors that happen in the parapharyngeal space are shown in the pie table. The most common tumor is Pleomorphic Adenoma which is a benign salivary tumor that has the potential to transform into a cancer. The pre-styloid space generally has tumors grow into it that start in the parotid gland. Infrequently, cancers are found here that either start in the parotid or spread from other parts of the body. The post-styloid space has mostly tumors that start from sensors on blood vessels (Paragangliomas) or tumors that start from the insulating cover of nerves (Nerve Sheath Tumors).
It is very difficult to biopsy the tumors in the pos-styloid space because they are immediately next to the carotid artery & jugular vein. The tumors in the pre-styloid space can undergo a biopsy using a thin needle when there is a safe window of access to the area; by that I mean when there are no other major structure getting in the way. Imaging studies such as MRI & CT scan will help us at the CENTER decide if your tumor is in a location where it can be safely biopsied.
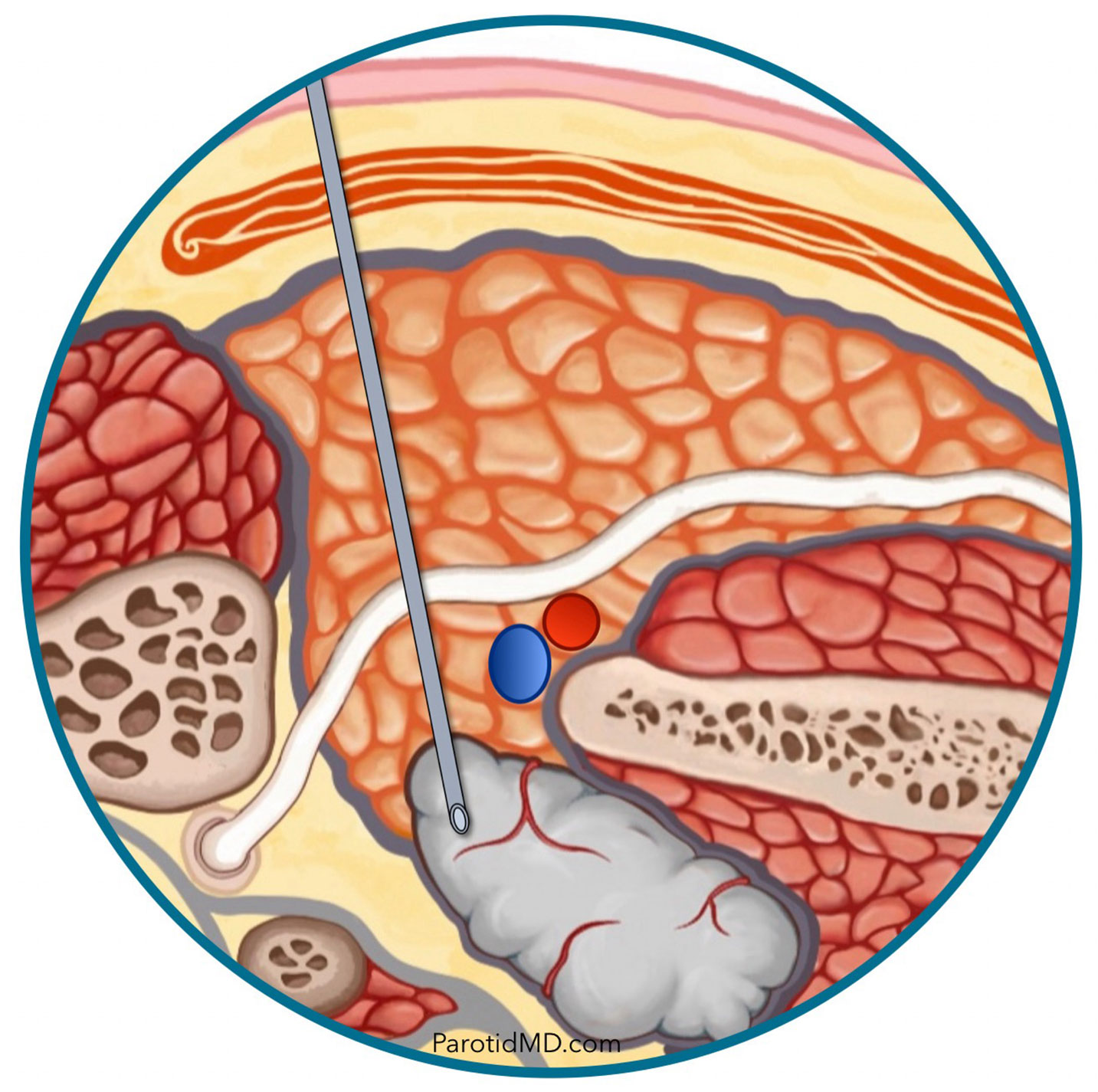
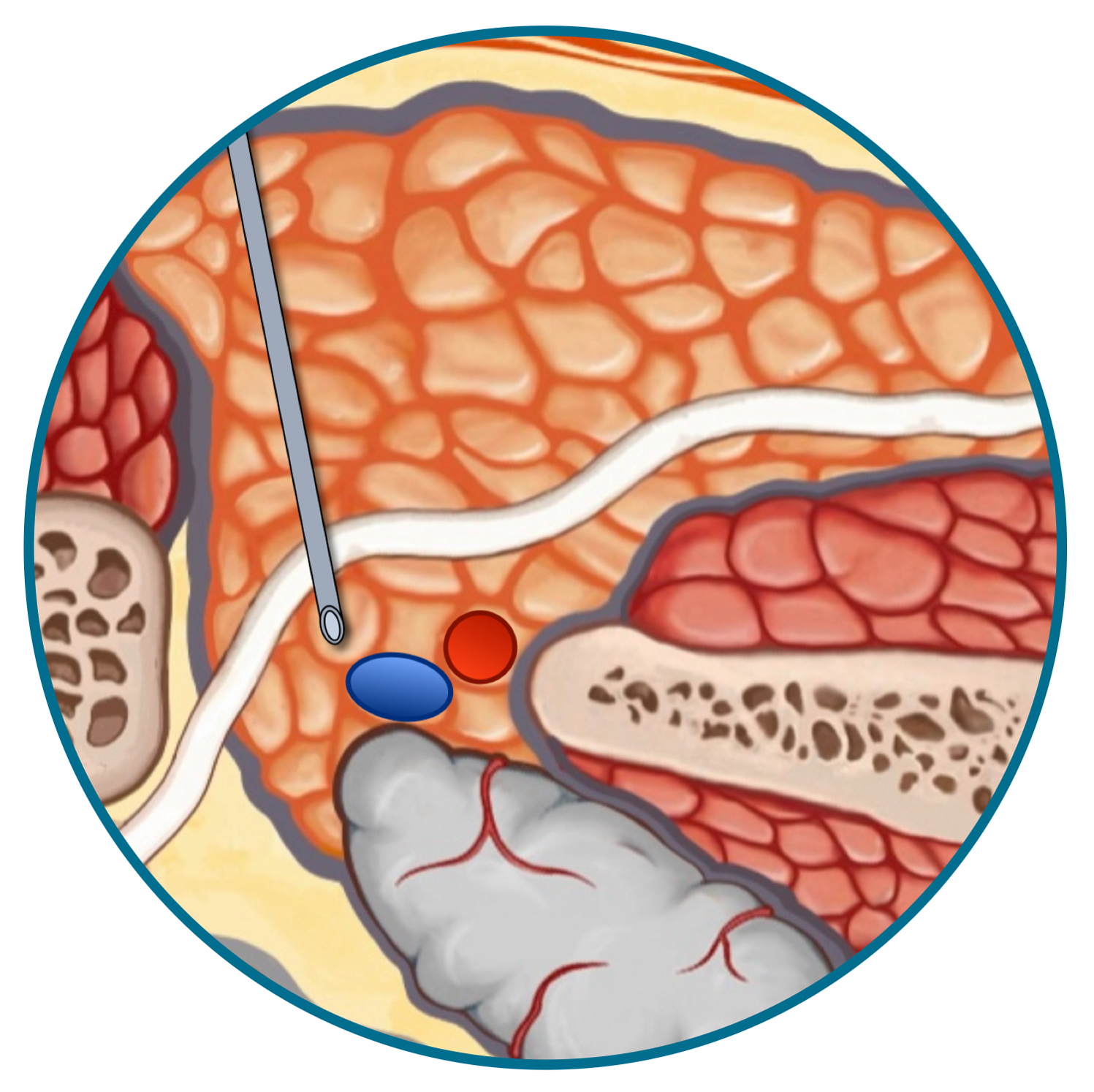
A small needle can be used with the aid of ultrasound or CT scan to perform biopsy on a deep lobe tumor, when there are no major structures blocking the path. The position of the tumor has to be such that the needle can be angled to avoid the facial nerve (shown below).
Larger tumors in the parapharyngeal space that are pushing against the throat may be biopsied with a thin needle through the mouth in the office.
Once the type of tumor is diagnosed with the needle biopsy. Then the appropriate treatment plan can be determined. The options can range from (1) monitoring in case of benign tumors that don’t have to potential to turn into cancer, and only remove when they show that they are growing on scans to (2) immediate removal based on pathology, size or symptoms. There are many different surgical approaches to the tumors in the paraphyarngeal space that will be discussed in the next section.
Surgical Treatment
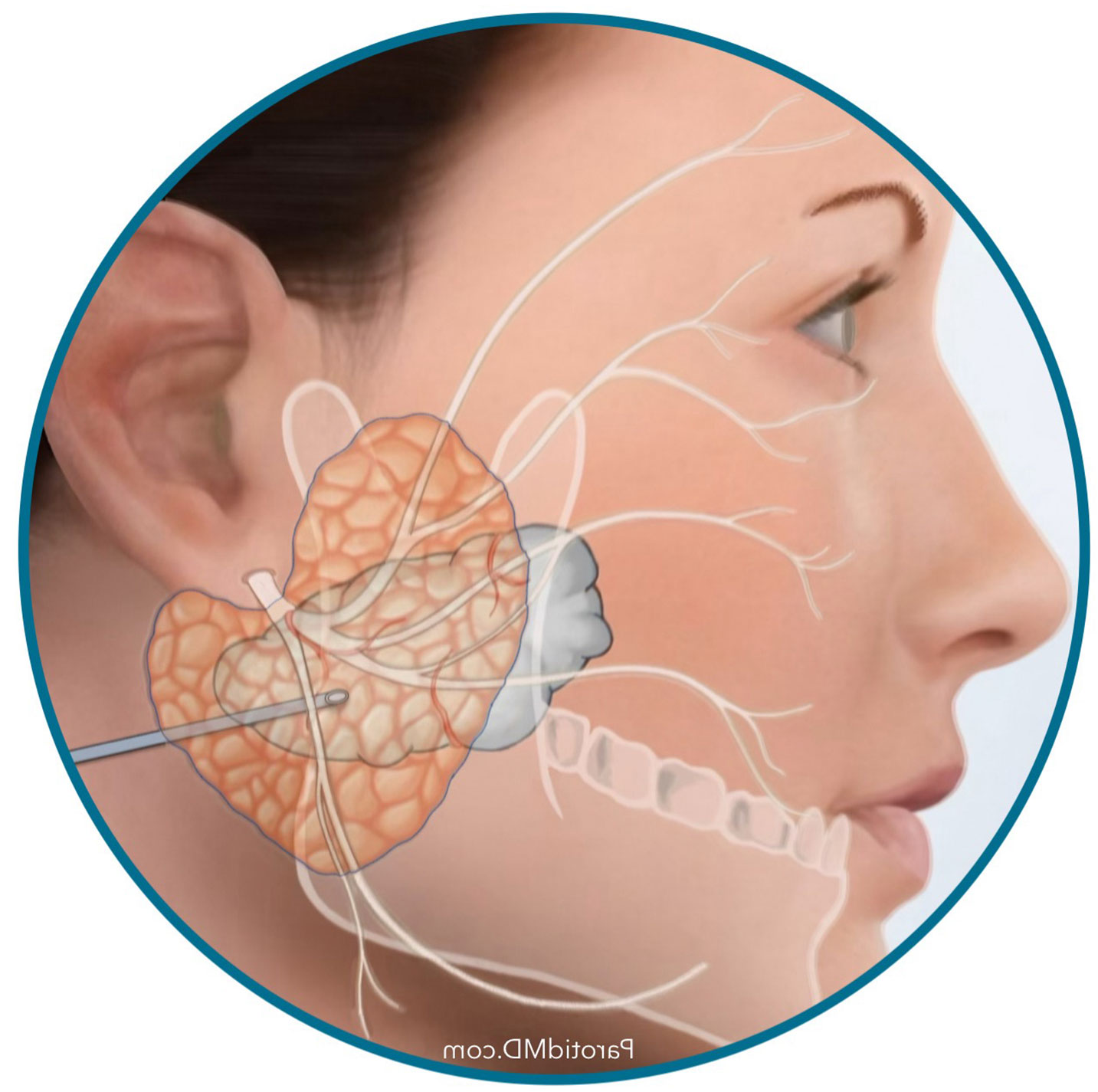
micro-paratidectomy approach
Deep lobe parotid tumors that are close to the facial nerve & extend into the parapharyngeal space need to be accessed through the microparotidectomy approach. This is so that the facial nerve branches are identified, preserved & protected before the tumor can be removed. This approach can also be called the trans-parotid approach which means through the trans-parotid approach, and the incision is the green line in front & behind the earlobe.
trans-cervical approach
Deep lobe parotid tumors that start from the tip of the deep lobe of parotid & extend into the parapharyngeal space but are not close to the throat or facial nerve can be removed through a small incision in the neck (Trans-cervical approach-Incision is the green line in the neck). This is because the tumor is far away from the facial nerve and does not require identification of the facial nerve to safely remove the tumor.
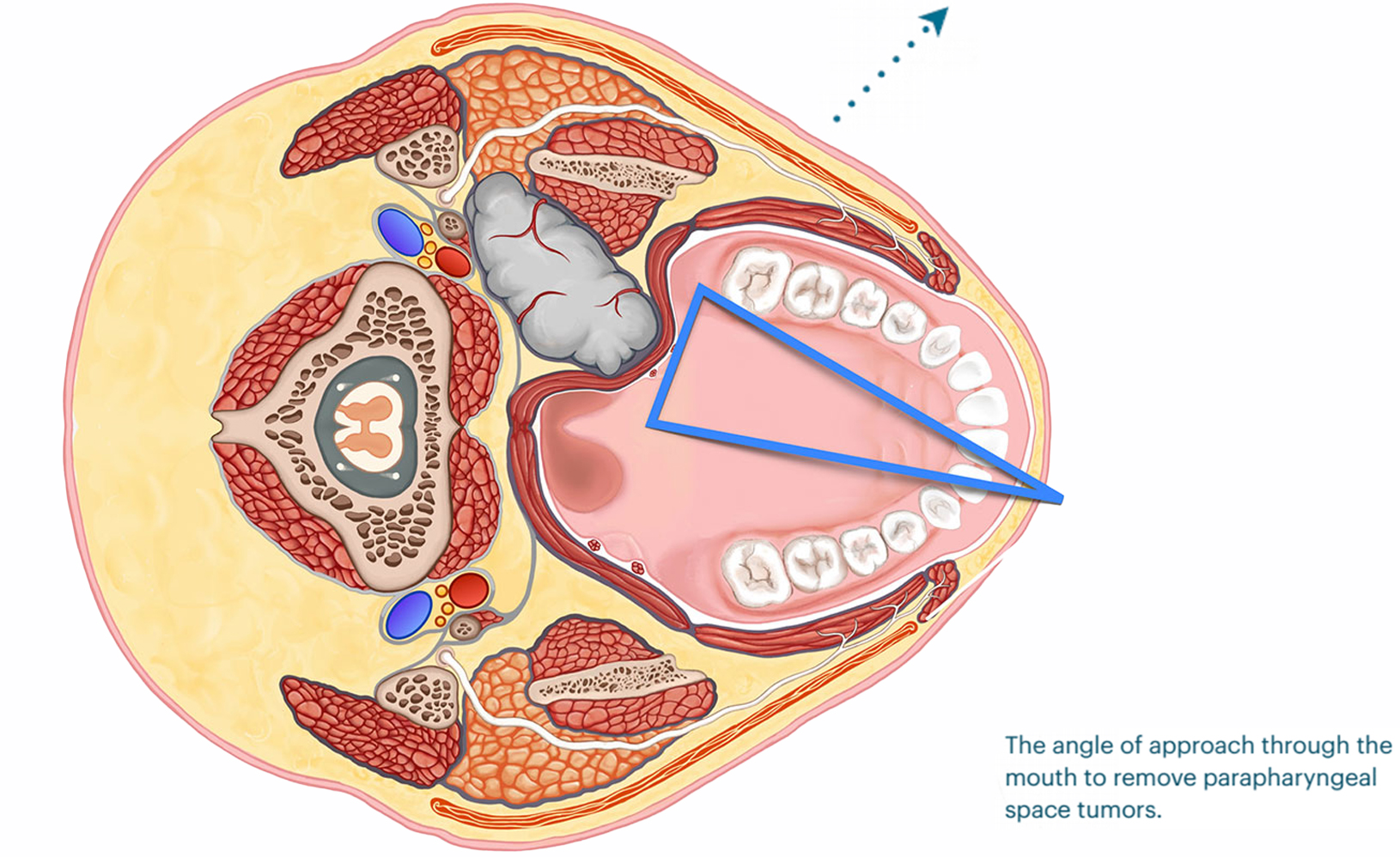
trans-oral approach
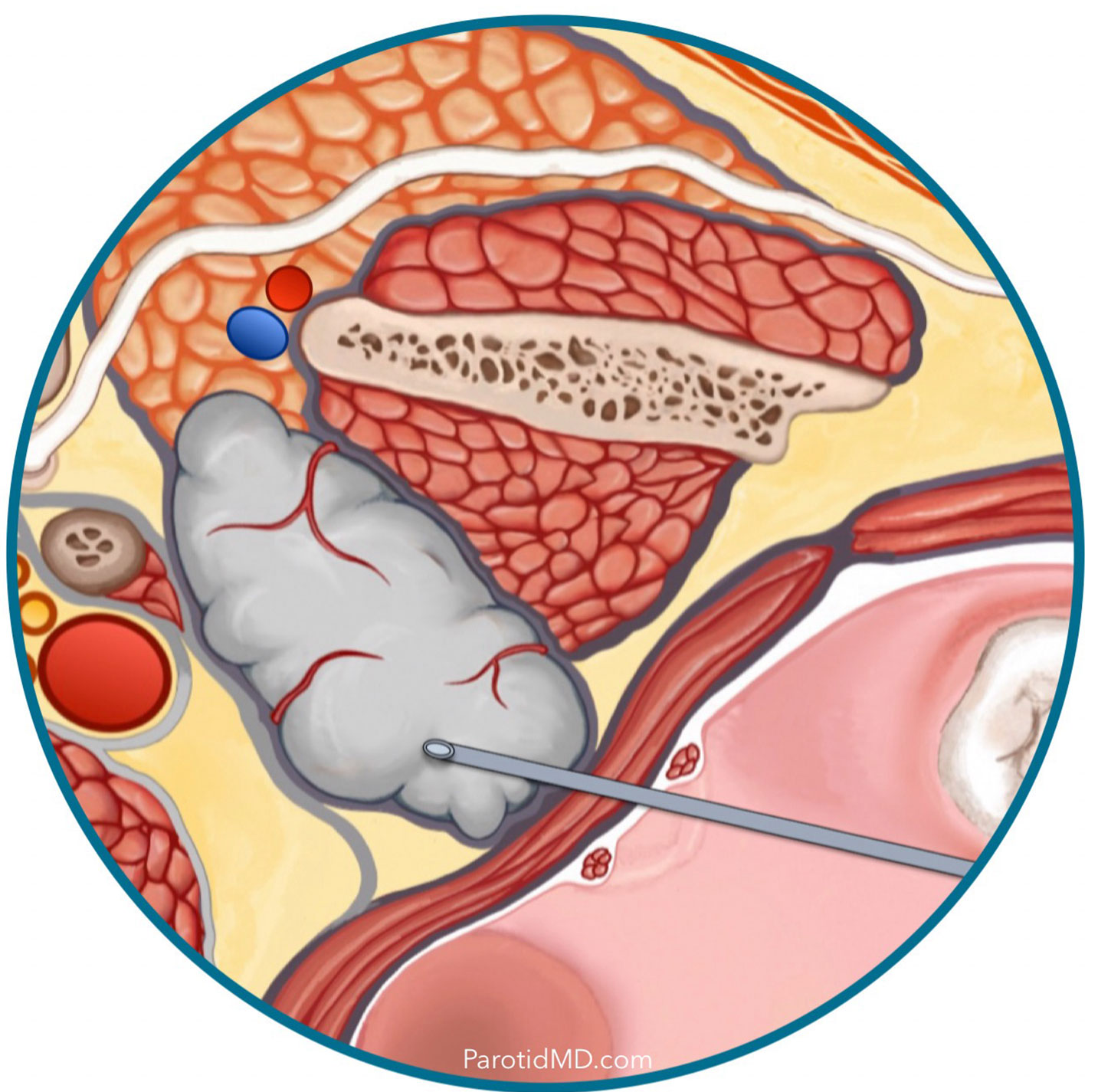
Parapharyngeal parotid tumors that originate from the deep tip of the parotid gland & grow to be close to the throat or bulge out into the throat can be removed through mouth (green line is the area of incision inside the mouth). This is possible because the tumor originates in an area that is a safe distance away from the facial nerve & can be immediately found through the mouth. If the tumor is much smaller or blocked by other structures in this space then it cannot be removed with this approach.
One of the 3 surgical approaches mentioned above can be used to remove a parotid tumor that has grown into the parapharyngeal space. The relationship to the facial nerve, the size and the anatomical extent of the tumor helps the surgeons at the CENTER determine which approach is most appropriate for you, safest for the facial nerve, best chance of removal of the entire tumor, and with the easiest recovery for you.
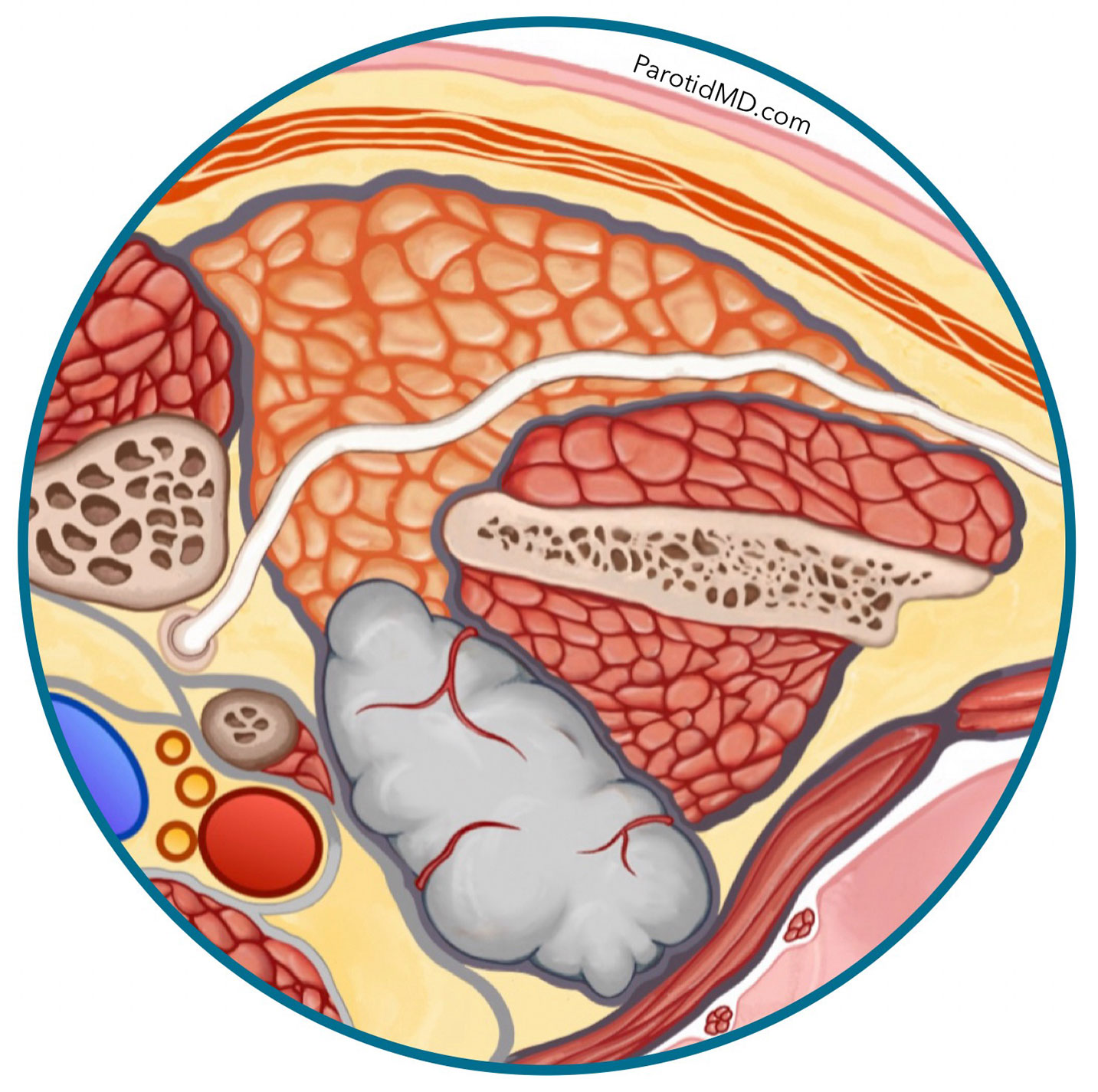
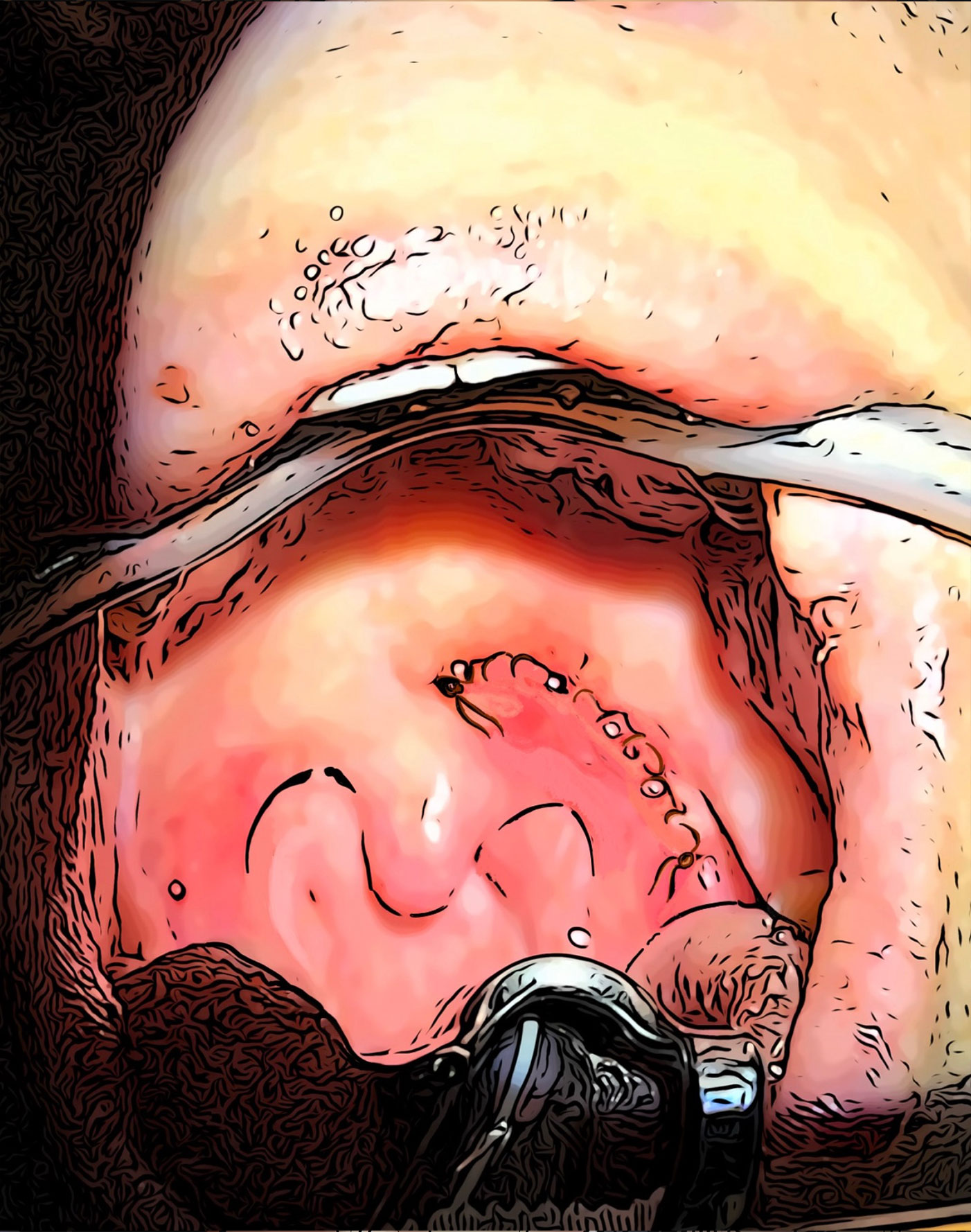
TRANS-ORAL PARAPHARYNGEAL TUMOR SURGERY
The parotid gland’s deepest most portion is behind and deep to the jawbone muscle. On occasion tumors start in this area and grow inwards. This area is confined by the jawbone (to the side), spine (in the middle) and the ear bone/Skull base (on the back), so the tumors that develop here can only grow in a forward direction which is towards the throat. Once they grow large enough they either get close to the mucous membrane of the soft palate (back of the roof of our mouth) or can push the palate in which case we can see a bulge in the palate when we look inside the moth.
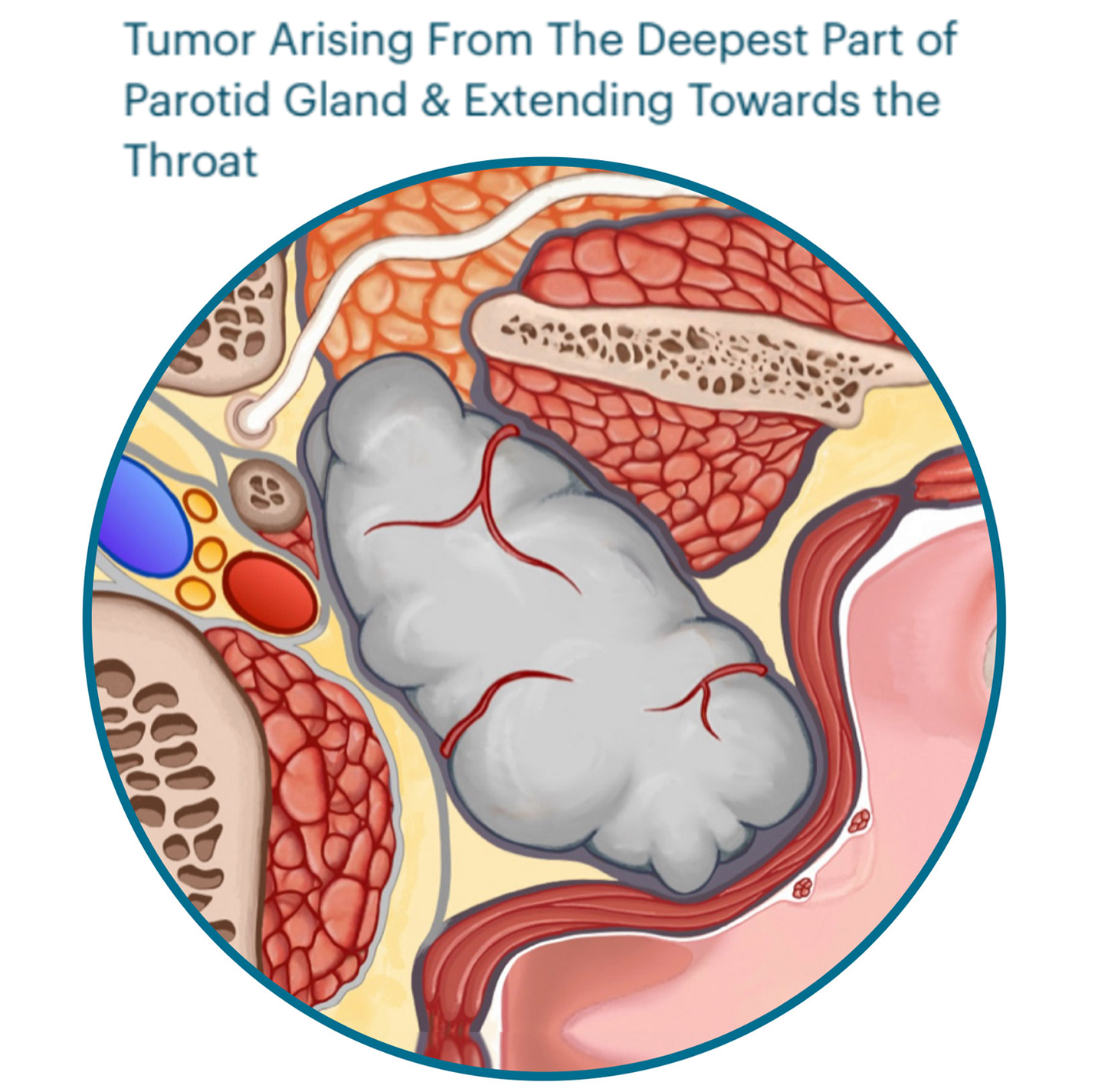
The parotid gland’s deepest most portion is behind and deep to the jawbone muscle. On occasion tumors start in this area and grow inwards. This area is confined by the jawbone (to the side), spine (in the middle) and the ear bone & the skull (on the back), so the tumors that develop here can only grow in a forward direction which is towards the throat. Once they grow large enough they either get close to the mucous membrane of the soft palate (back of the roof of our mouth) or can push the palate forward which can be seen as a bulge in the palate when we look inside the mouth.
TRANS-ORAL PARAPHARYNGEAL TUMOR SURGERY
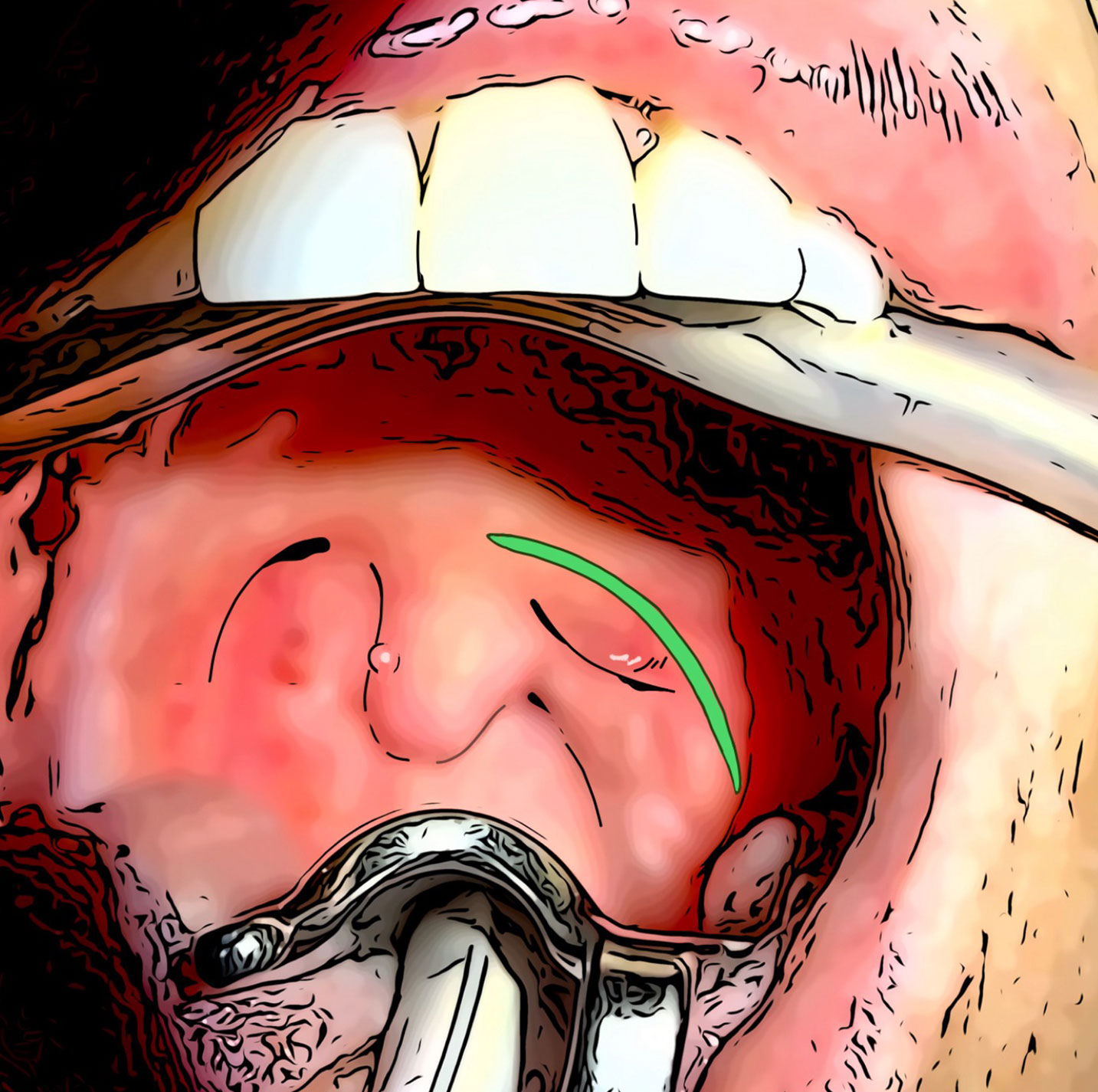
Live Surgery Transformed into Animation
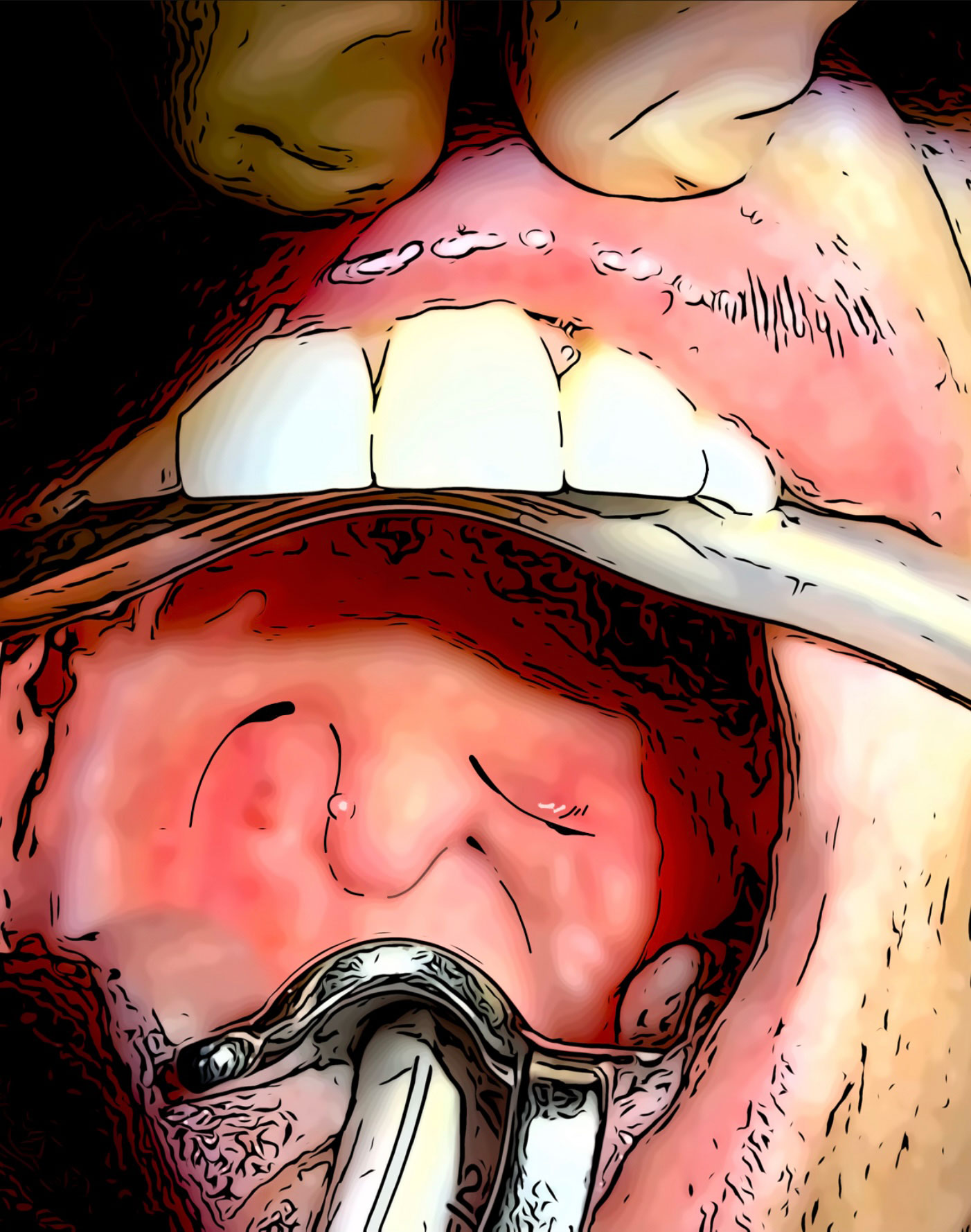
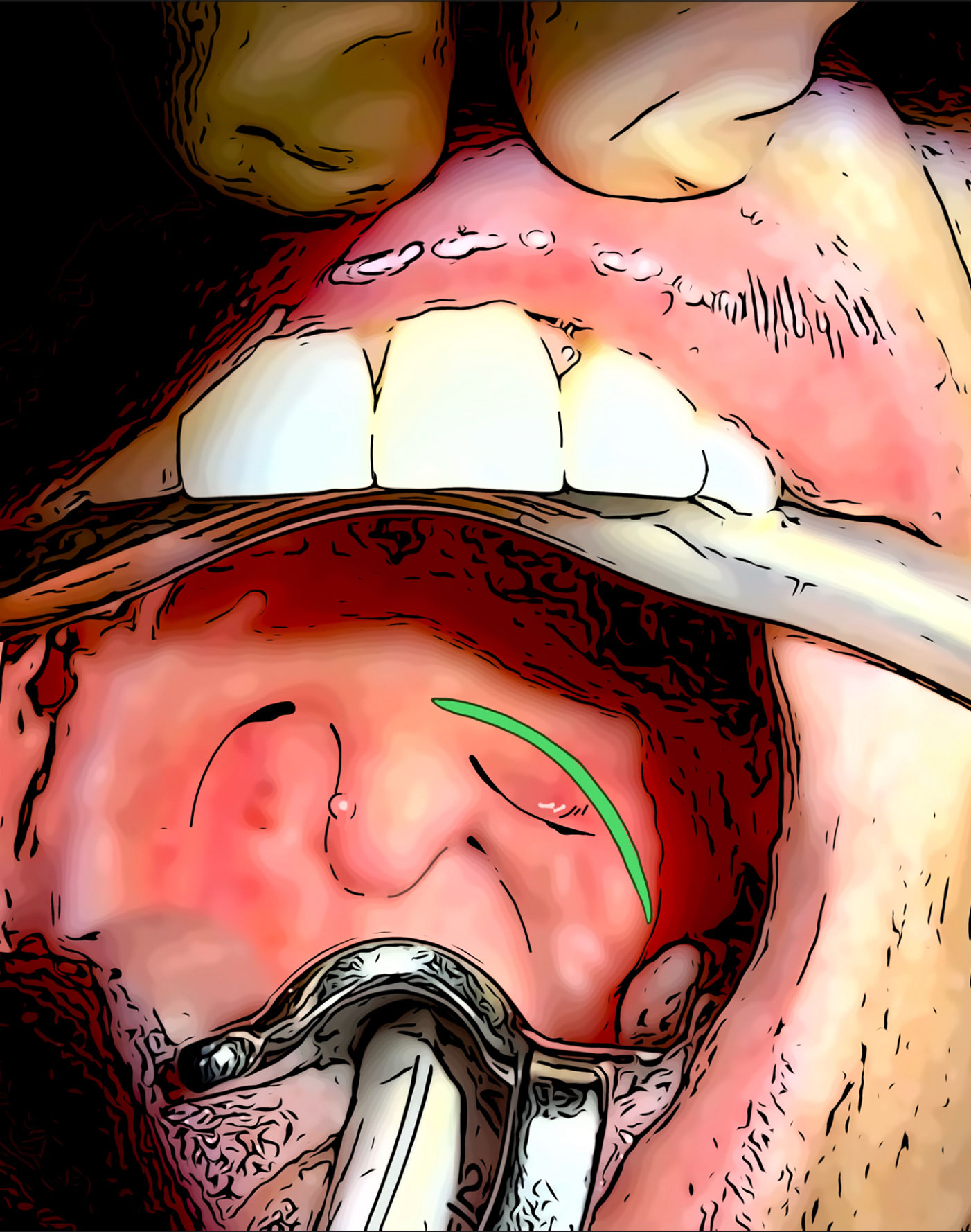
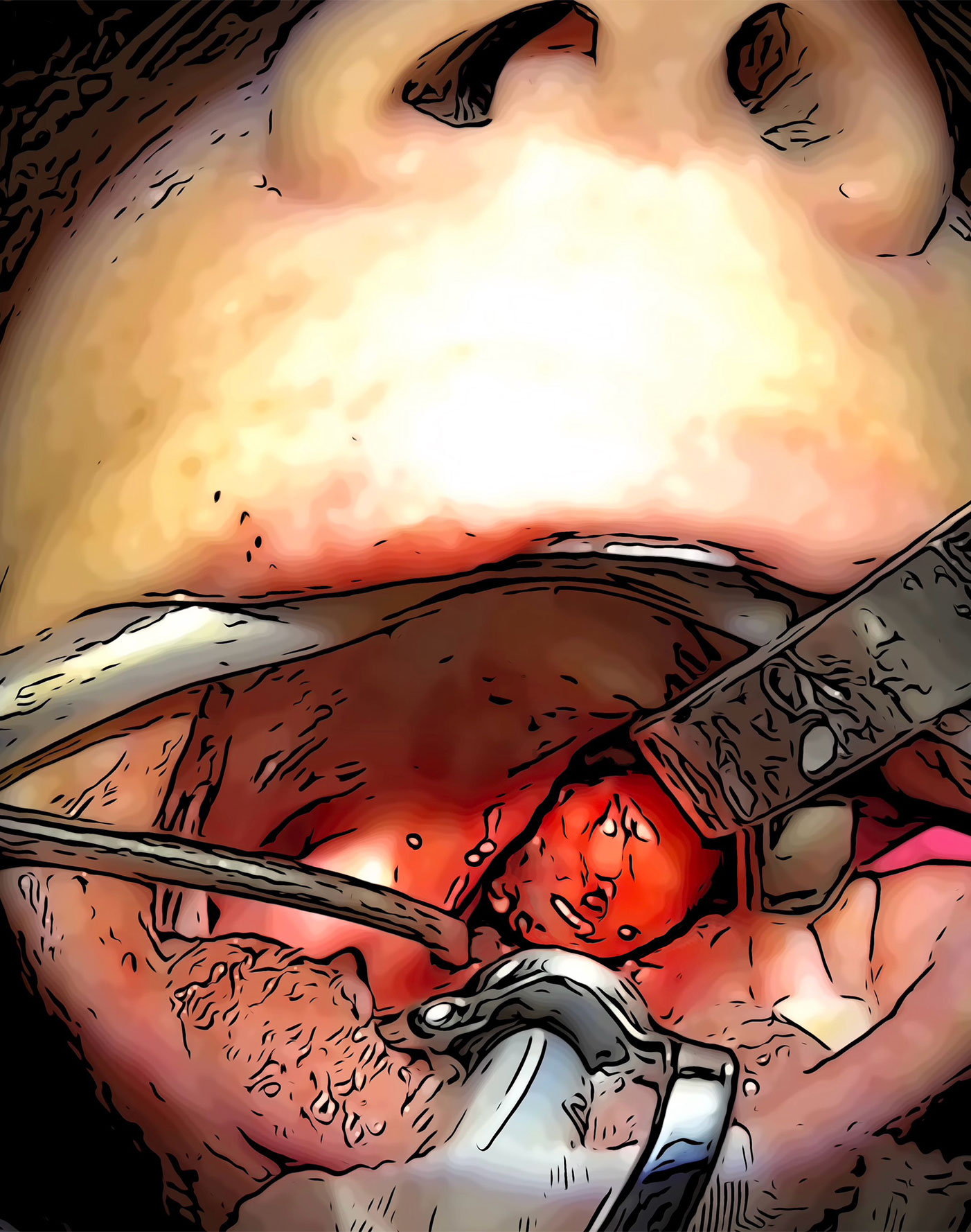
The incision (green line) is made on the palate. The tumor can be immediately seen. It is carefully separated from the surrounding fat & muscles. In case of benign tumors, since the tumor has both it’s own capsule & the capsule of the parotid gland is covering the tumor no additional tissue needs to be removed around it. Once the tumor is freed on all sides it may be removed. The video below shows the removal of the tumor through the mouth.
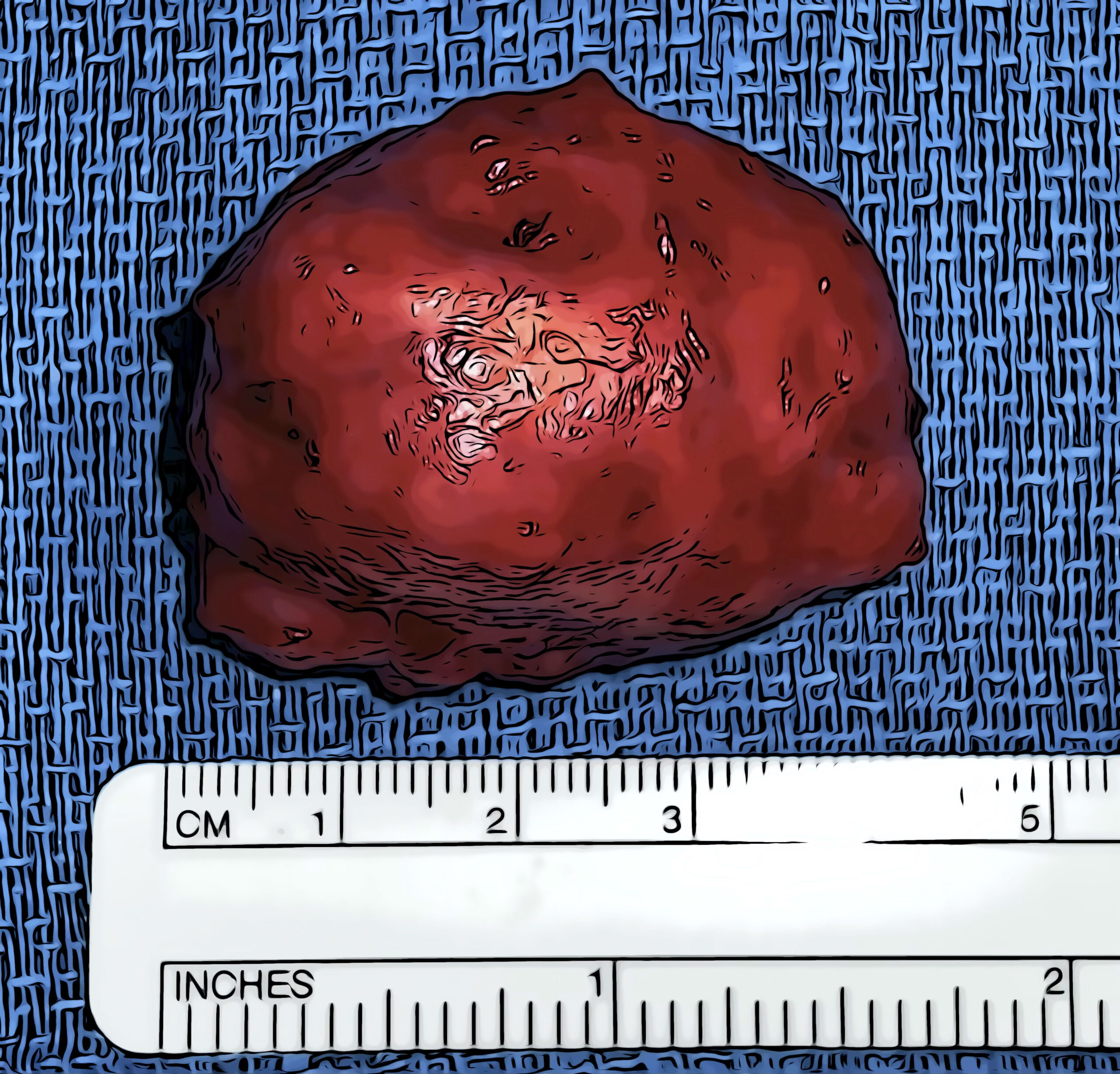
The incision is closed in multiple layers with absorbable sutures. These sutures don’t have to be later removed. The tumor is thoroughly inspected, once removed. The capsule surrounding the tumor is also checked. The tumor may be sent to the pathologist during surgery for immediate examination to see what type it is. This is done if the tumor has not been already biopsied prior to the operation, or if it has suspicious features (areas that are very hard, or has roots attaching it to the muscles etc.). This usually takes 20 minutes, and the results called into the operating room.
FREQUENTLY ASKED QUESTIONS
Does parapharyngeal space tumor removal need to be performed at a hospital, and does it require overnight stay at the hospital?
NO. This is an outpatient procedure for the majority of patients that can be done at an outpatient surgery setting. The only exceptions are patients who have other medical problems such as heart, lung or kidney disease that requires more medical attention and monitoring for these particular organs rather than the parotid surgery itself.
Are the facial nerves monitored during parapharyngeal space
parotidectomy?
Yes, in every single case a facial nerve monitoring system is used.
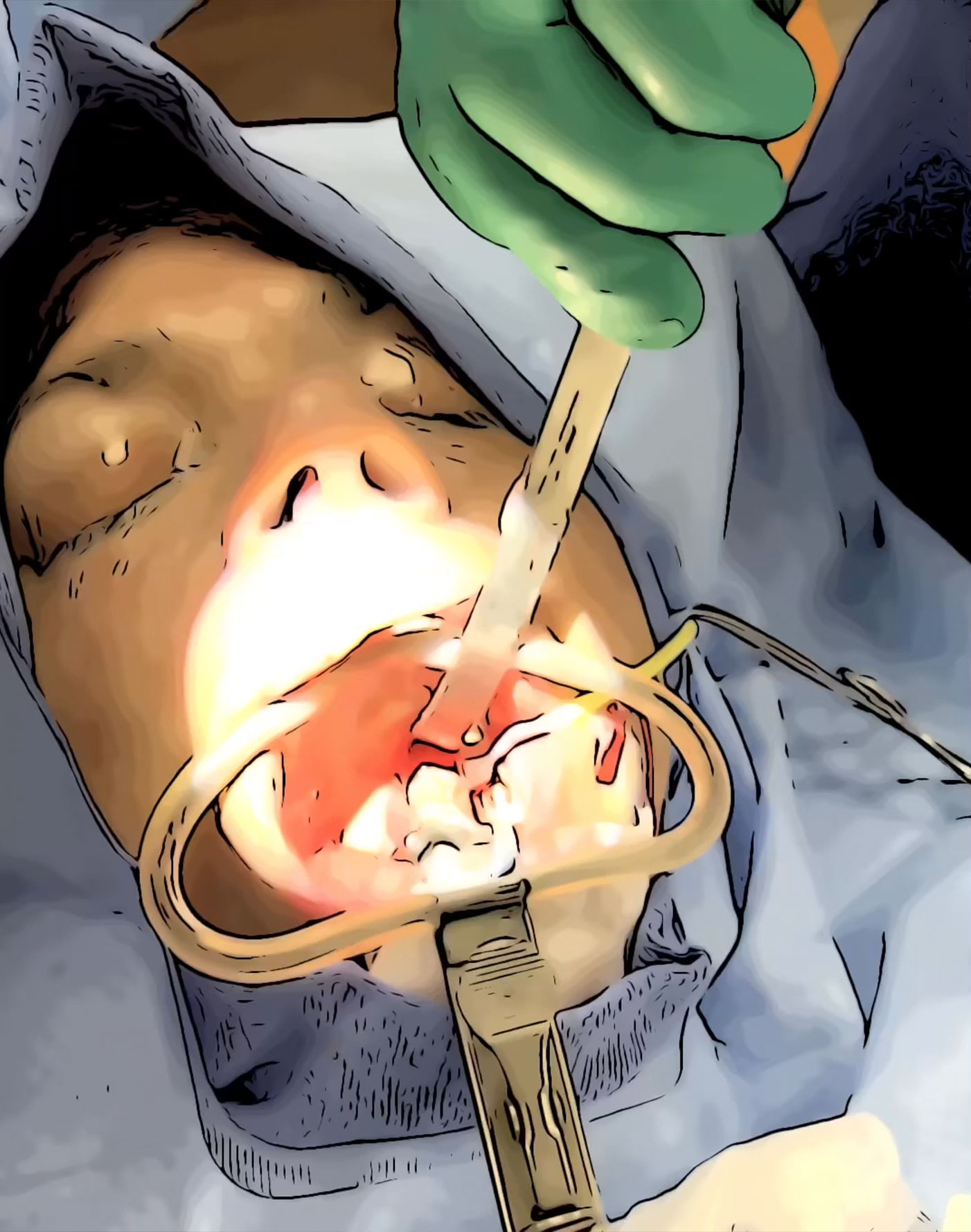
This system continuously checks the activity of the facial nerve. When
it senses the slightest activity close to the nerve it sends alerts. It alerts the surgeon that they are close to the nerve and to exercise extreme caution. This is no substitute for expertise but is an additional measure of safety for the nerve. In the video the monitors can be seen as blue probe, next to the eye & red probe for the lip.
In case of trans-parotid or micro-parotidectomy approach, because the
facial nerve branches are identied, during surgery the facial nerve
may be stimulated to identify the nerve location. And after tumor
removal it may be stimulated to conrm all branches are working and
unharmed.
STIMULATION OF THE FACIAL NERVES AFTER REMOVING THE TUMOR TO ASSURE ALL BRANCHES ARE WORKING (converted into animation)
Are parapharyngeal space parotid tumors more likely to recur or come back?
Interestingly benign tumors in this area tend to come back less often. It is perhaps because the tumor has its own capsule (cover) but also the capsule of the parotid gland itself (double capsule). Of course, the expertise of the surgeon is an important factor. The tumors are the same in terms of aggressiveness of behavior in the superficial the deep lob & parapharyngeal space. However, access is more limited in the parapharyngeal space which makes the experience of the surgeon be of utmost importance.
Are the tumor in the parotid deep lobe & parapharyngeal space more likely to be cancerous?
Fortunately not. Close to 80% are benign just like the rest of the parotid gland areas. Only 20% are cancers.
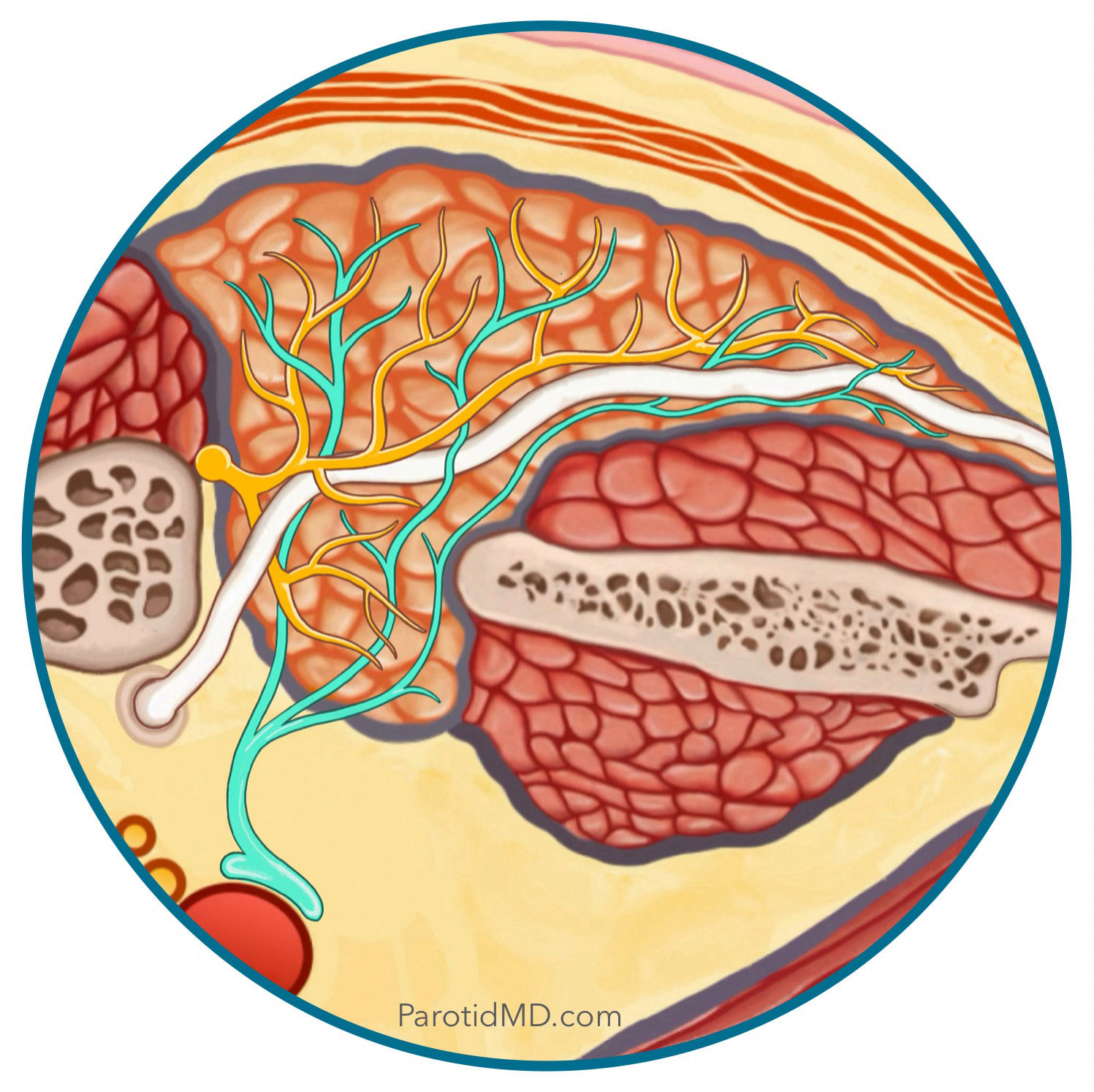
What is First Bite Syndrome?
Besides the facial nerve there are 2 other much smaller nerves that come into the parotid & control production and release of saliva. One set of microscopic nerve branches come from Auricotemporal Nerve that tell the gland to produce & squeeze out saliva (dark yellow); the other are set of very small nerves that come from the area deep to the parotid gland (light green – Sympathetic Nerve branches that travel with the carotid artery) and come in the gland and counter act the effects of the Auricotemporal Nerve. So the two nerves balance each other. If a tumor in the deep lobe either involves the Sympathetic Nerve branches or if during surgery a lot of these nerve branches are removed along with the tumor, then the Auricotemporal Nerve works with the counterbalance of the Sympathetic Nerves and therefore cause the parotid gland to squeeze hard during the first bite of the meal. The pain is instantaneous and stops with the rest of the bites of the meal. In most cases, this problem resolves over time.
Is Frey’s syndrome common after removal of parapharyngeal space tumors?
It depends on which approach is used to get to the parapharyngeal space; trans-oral & trans-cervical approaches do not allow for Frey’s syndrome to occur, however, there is a chance with micro-parotidectomy approach if a an appropriate reconstruction is not done. Fortunately, here at the CENTER a reconstructive procedure is always done for parotid surgery that have the risk of Frey’s syndrome.
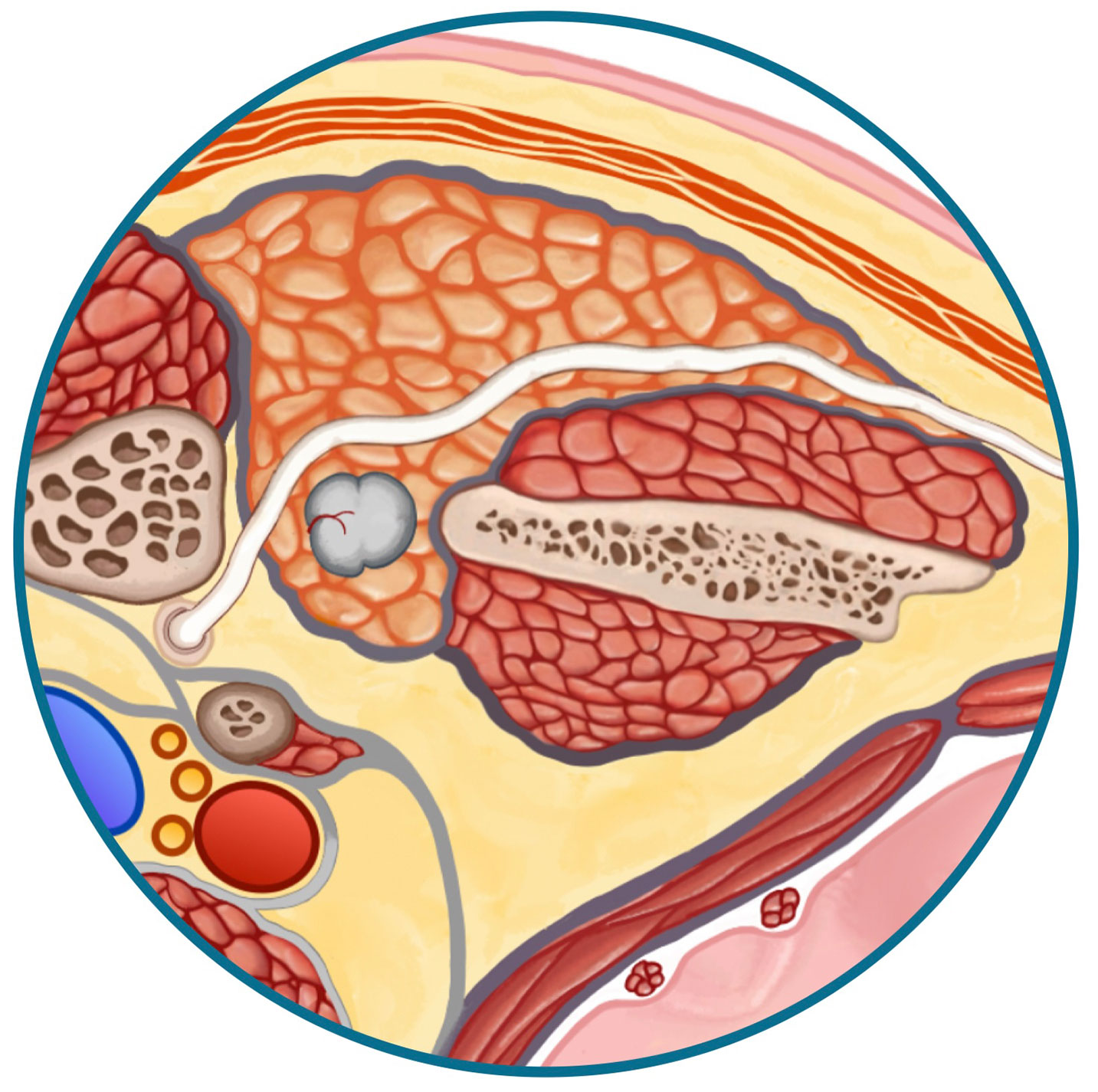
Can a needle biopsy be done on all parapharyngeal space tumors?
Not always, and it has to do with other possible anatomical structures blocking the passage of the needle. In the picture to the right, large blood vessels in the deep lobe of the parotid gland obstruct the way for a needle to be able to safely get to the tumor and get a biopsy. When this occurs, the doctors at the CENTER will depend on the the shape, configuration, size and behavior of the tumor to determine wether it is benign or cancerous. This is of course not as certain as a biopsy, but can be helpful in the hands of an experienced parotid specialist.
How are most of the parapharyngeal space tumors identified?
Great majority are found incidentally when a CT scan or MRI is done for another reason, for example a brain scan being done for headaches may show a tumor in this area. The reason for the accidental finding of these tumors is that the are usually without symptoms.
What are the risks of trans-cervical parapharyngeal
tumor removal & how is the recovery?
When the surgeons at the CENTER elect to do a trans-cervical paraphayrngeal space tumor removal, it is because the tumor is far away from the area of the facial nerve. Since there are no other major structures in the pre-styloid parapharyngeal space the risks are minimal.
The incision as shown in the image to the right (encircled in green) in the natural crease lines of the neck and heal very well. This approach actually has a much easier recovery as compared to trans-oral or trans-parotid. It is an outpatient surgery, and the person can immediately eat a normal diet. Since there is no need for a reconstruction and the inside of the mouth is untouched the recovery is fairly simple and one can get back to routine activities much more rapidly.

Is Robotic Surgery appropriate for parapharyngeal space parotid tumors, and is it more likely to recur or come back with robotic surgery?
Those surgeons who perform trans-oral Parapharyngeal tumor surgery were very excited when the the surgical robots became available. However, the robot’s arms does not allow the surgeon to feel how hard or soft the tumor is, as such when the robot grasps or holds the tumor, often times it ruptures the tumor. Rupture of the tumor surface is a big problem, because it can cause tumor cells to spill into the wound. In time, those spilt tumor cells will grow and create multiple recurrences. As such, most experienced surgeons have stopped using the robot in this area.
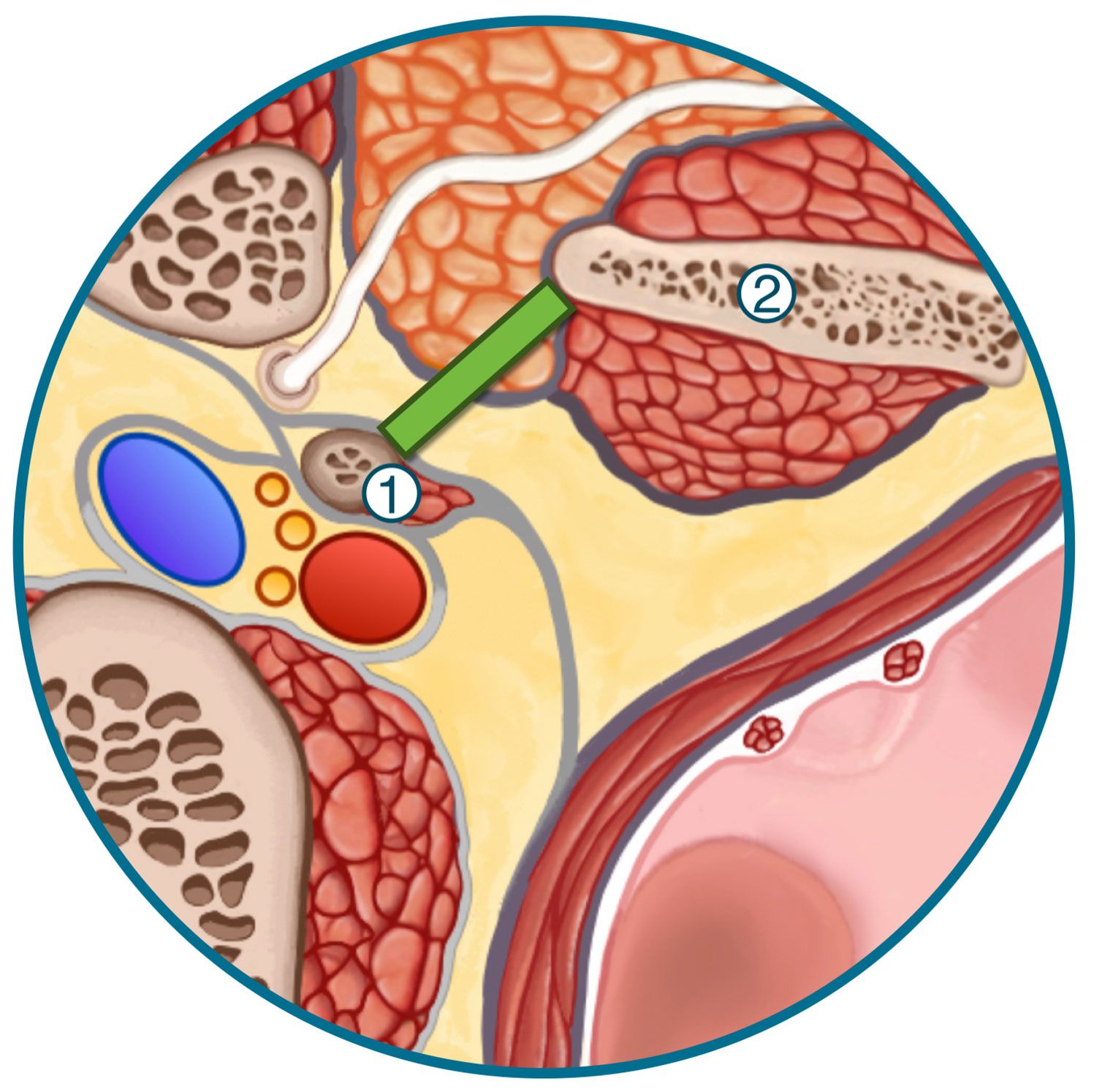
What is the Stylomandibular Tunnel?
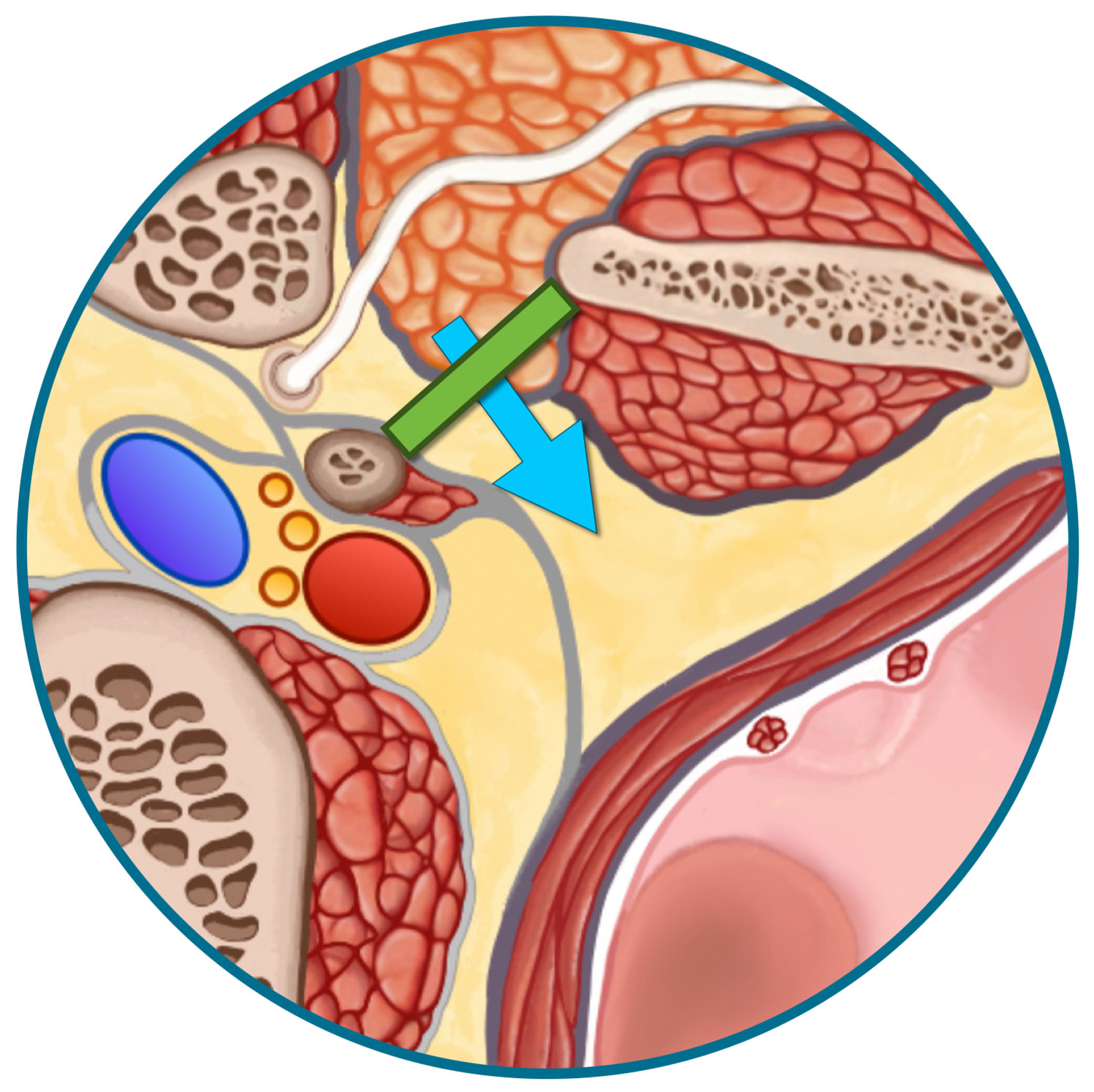
There is space between the jawbone (mandible) marked as (1) and the styloid bone (2). This gap between the two bones is called the stylomandibular tunnel (the green line). The deepest portion of the parotid gland sits here. When tumor start in the deepest tip of the parotid gland and grow, they pass through this tunnel to get into the parapharyngeal space (the blue arrow).
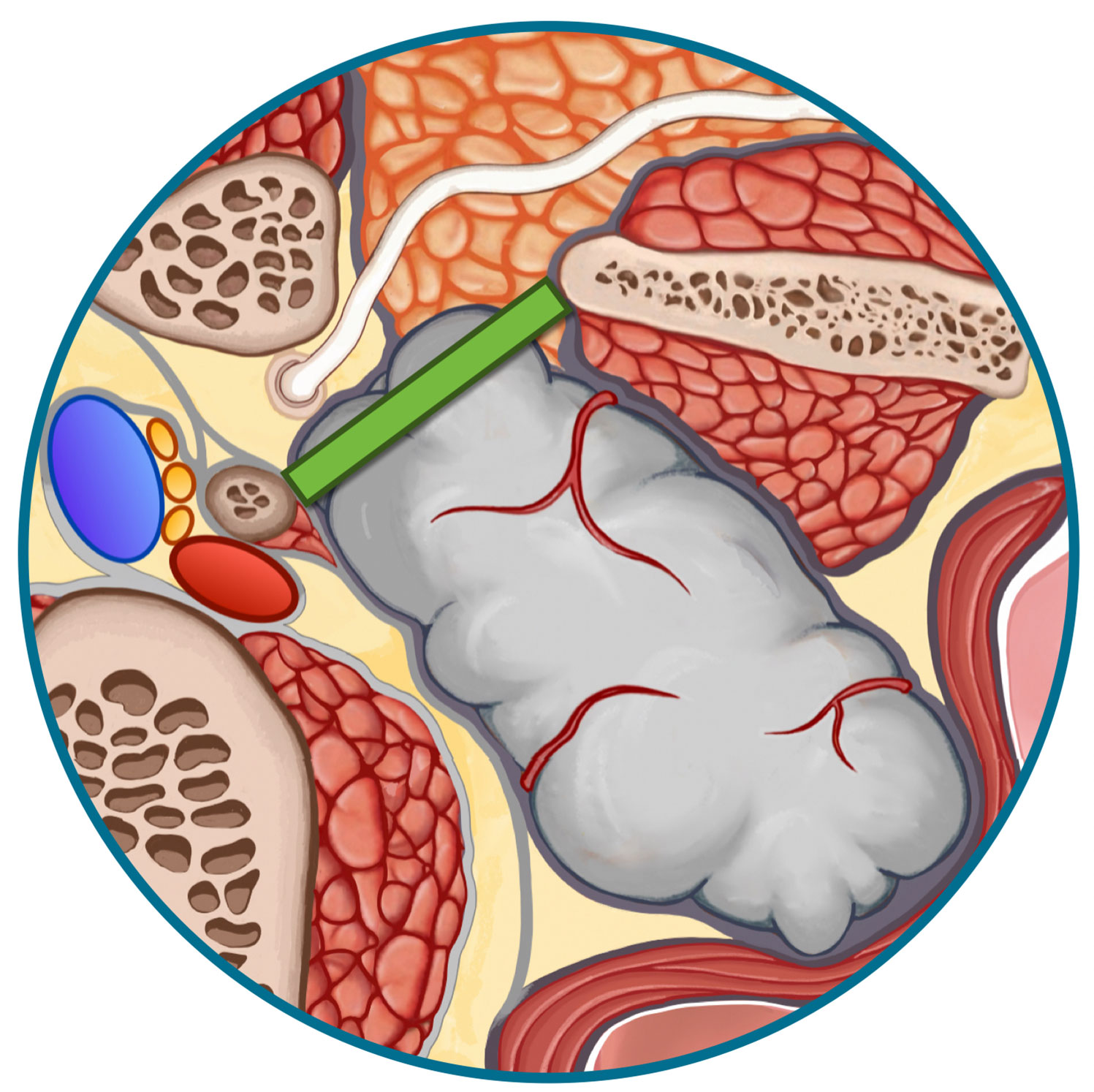
Sometimes, when a tumor that is growing into the parapharyngeal space gets large it pushes on the jaw bone but also more so on the styloid process (which is much smaller). This can widen the stylomandibular tunnel; which is an indication of note only a large size of tumor but also that the tumor has been present for a while to reshape and reposition styloid bone (image below).

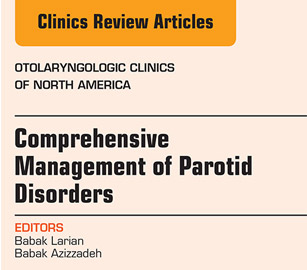
Meet The Team
Led by board-certified parotid surgeon, Dr. Babak Larian, our team of specialists has decades of experience successfully diagnosing and treating diseases of the parotid glands with minimally invasive procedures. Distinguished by our compassionate care and cutting-edge techniques, the CENTER has developed a reputation for delivering the best parotid tumor surgery available.