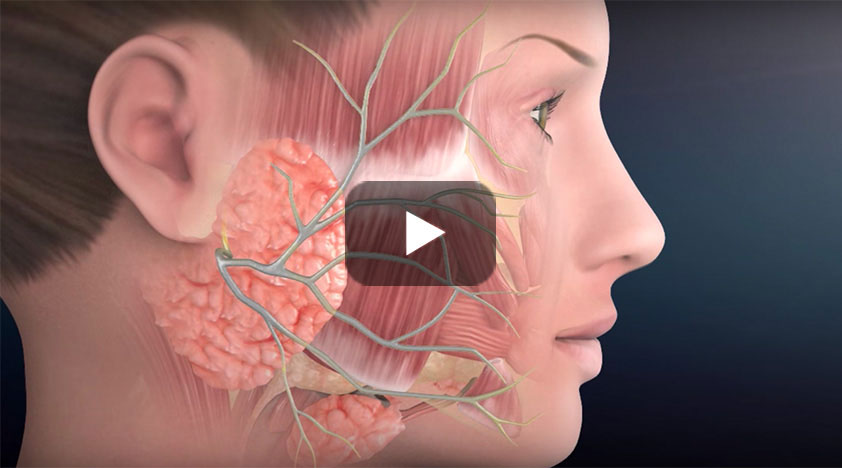
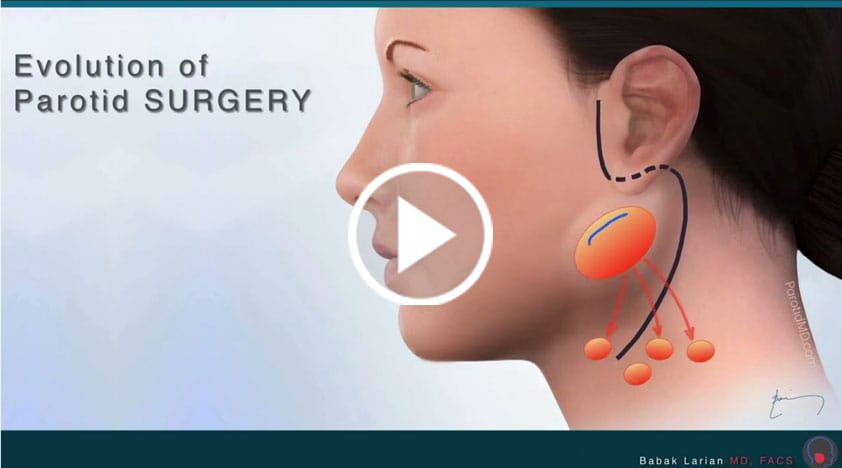
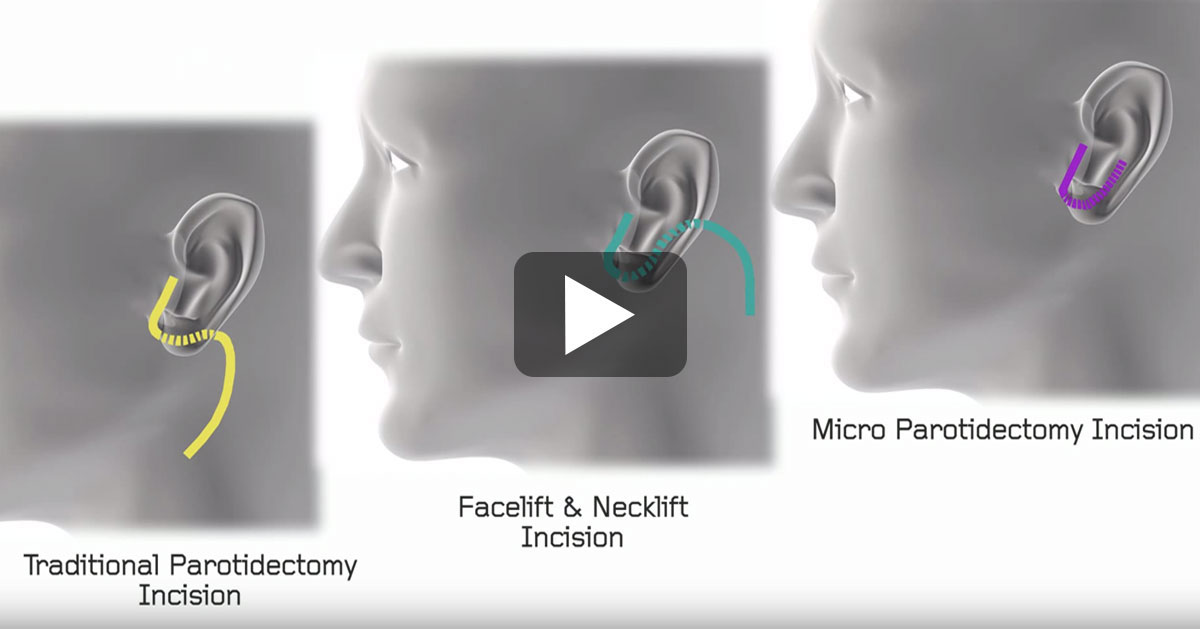
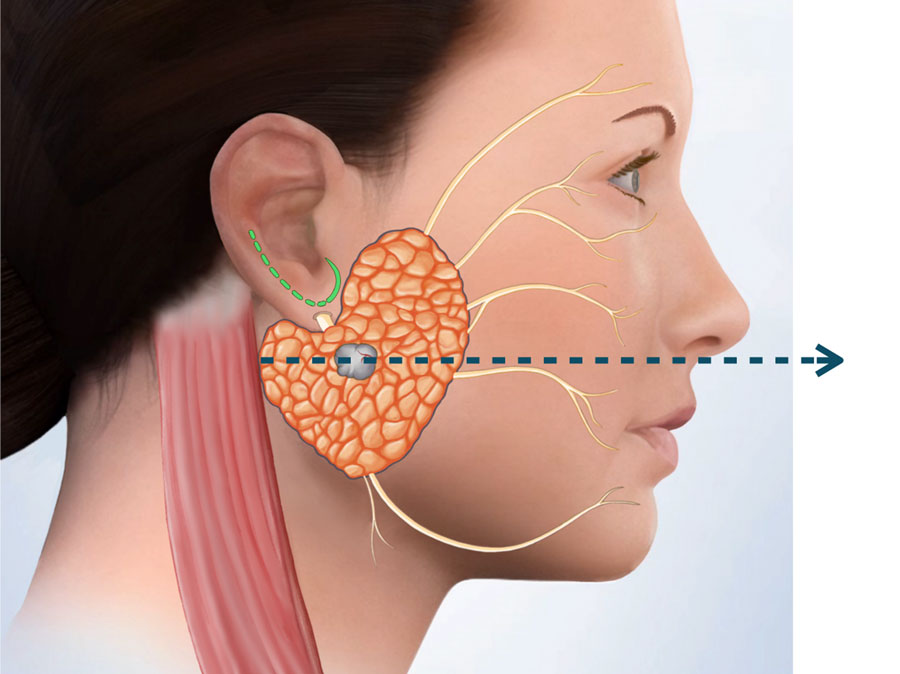
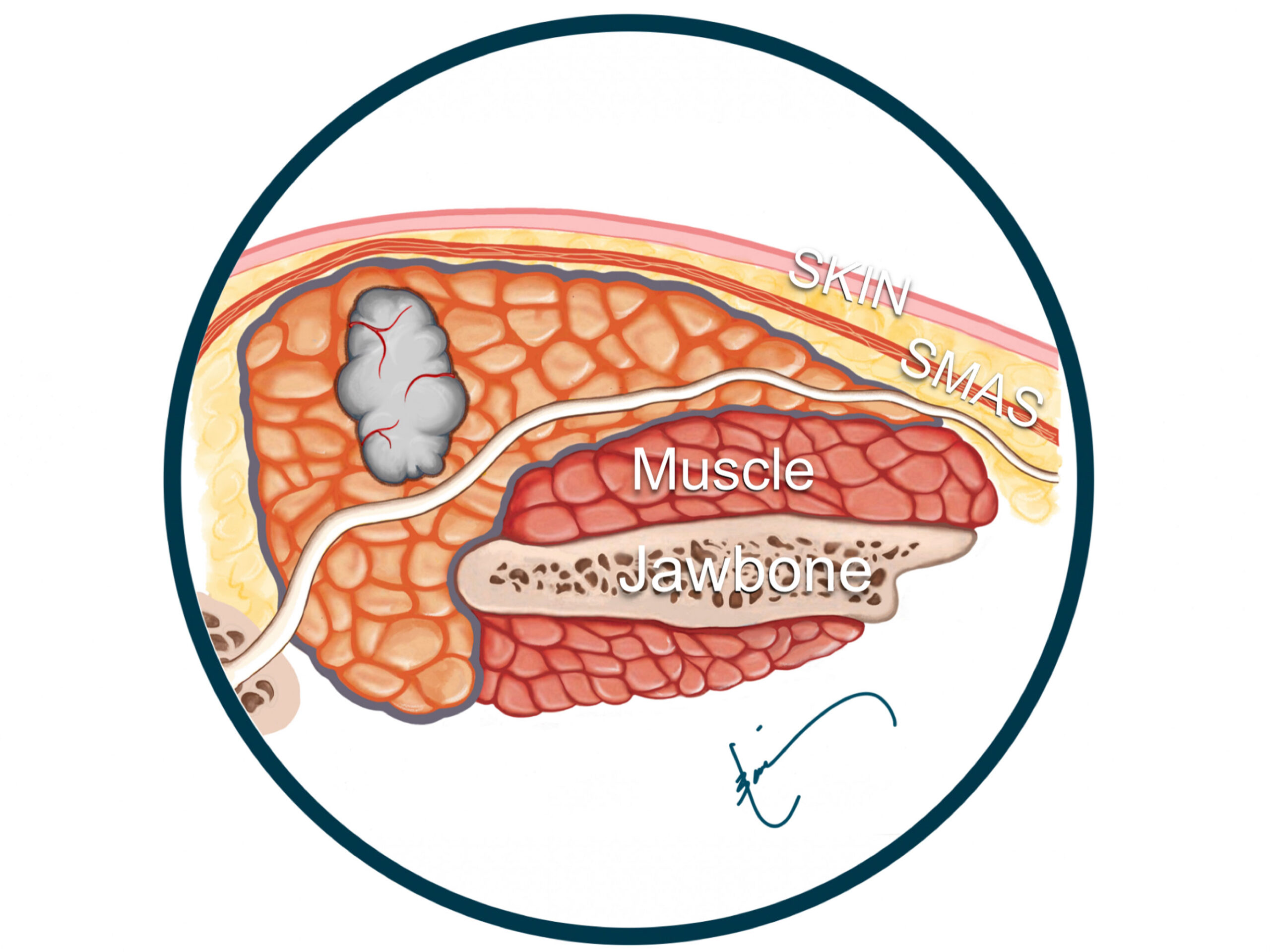
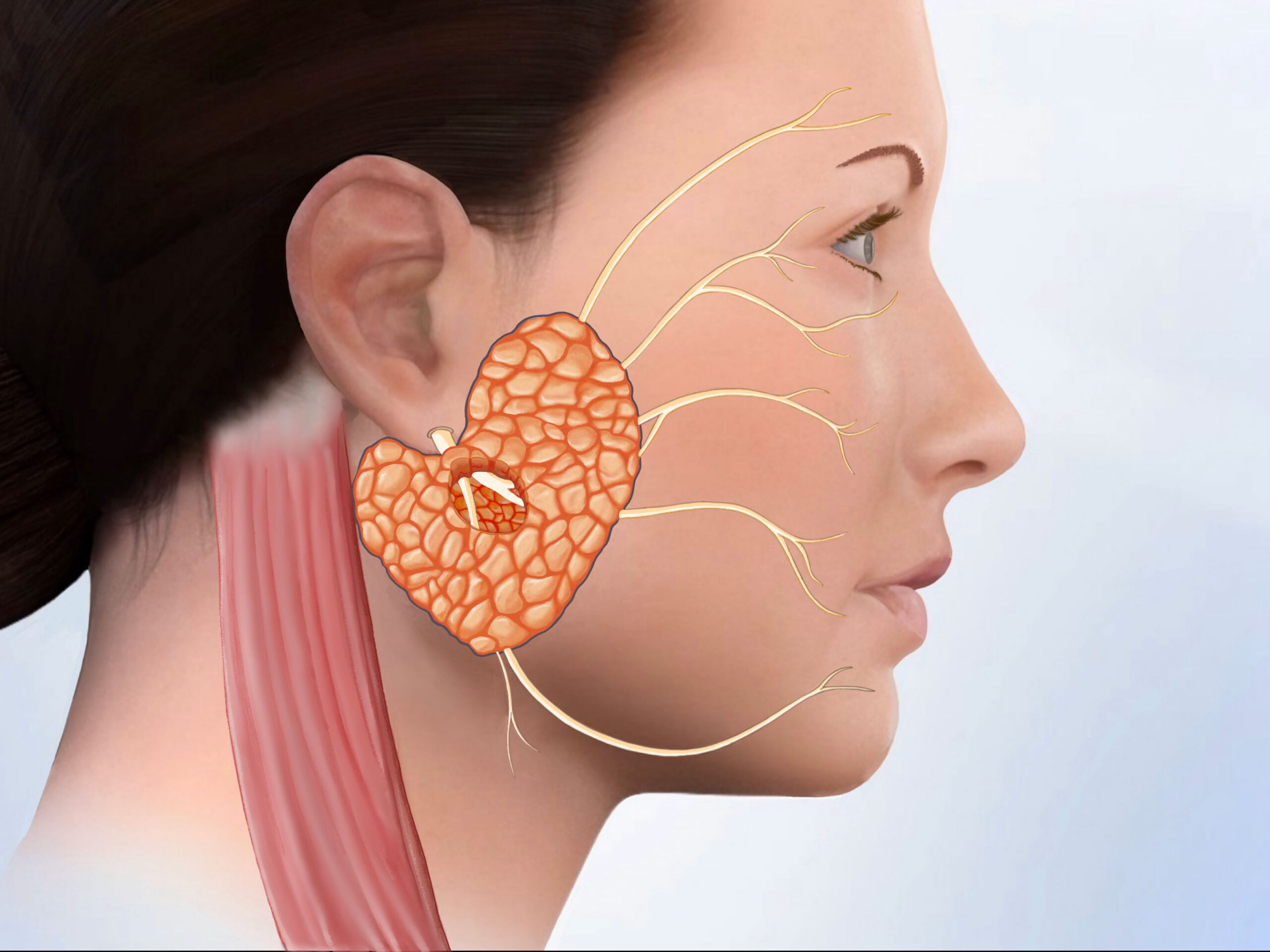
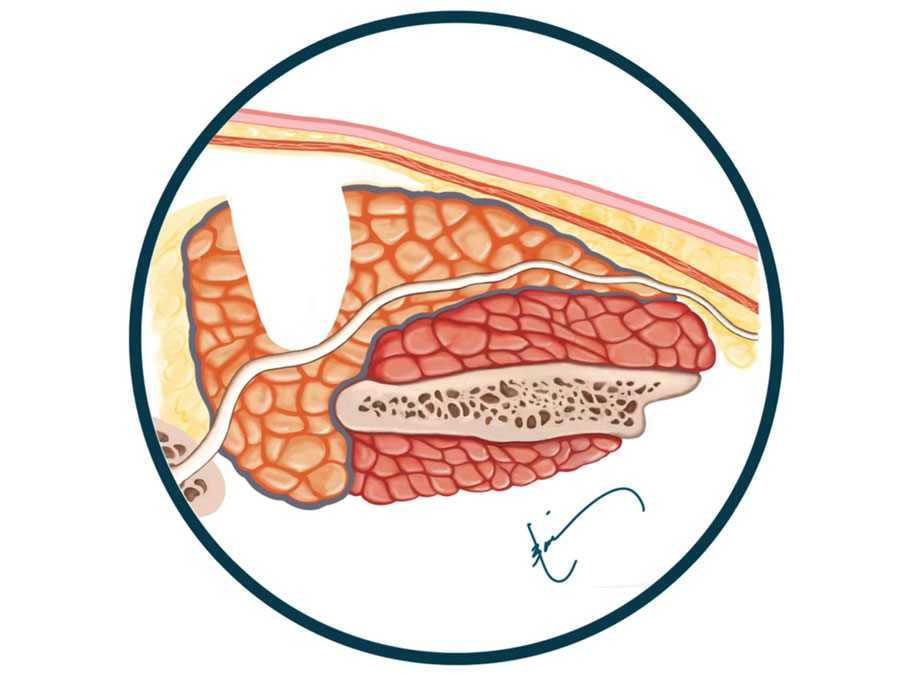
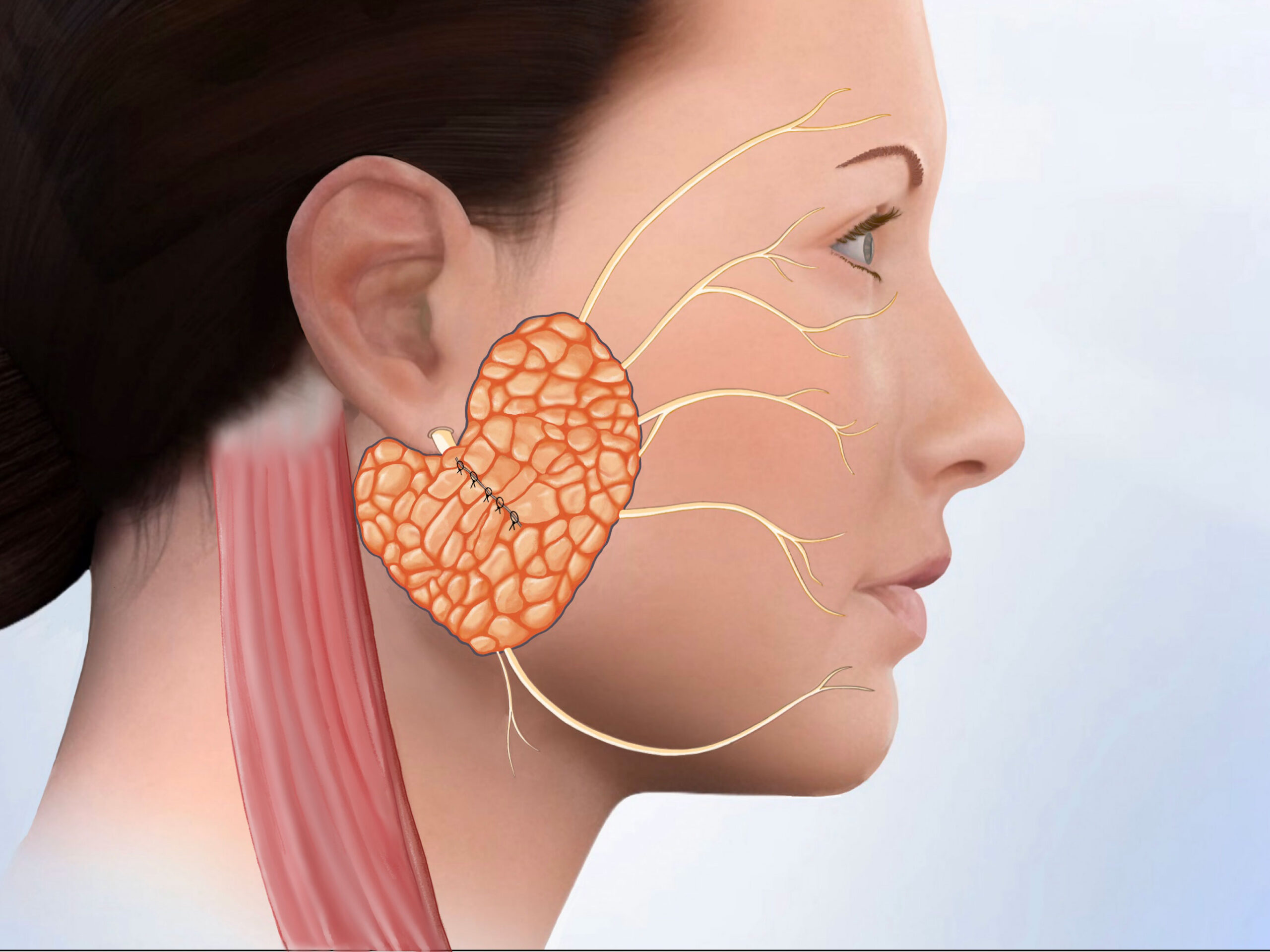
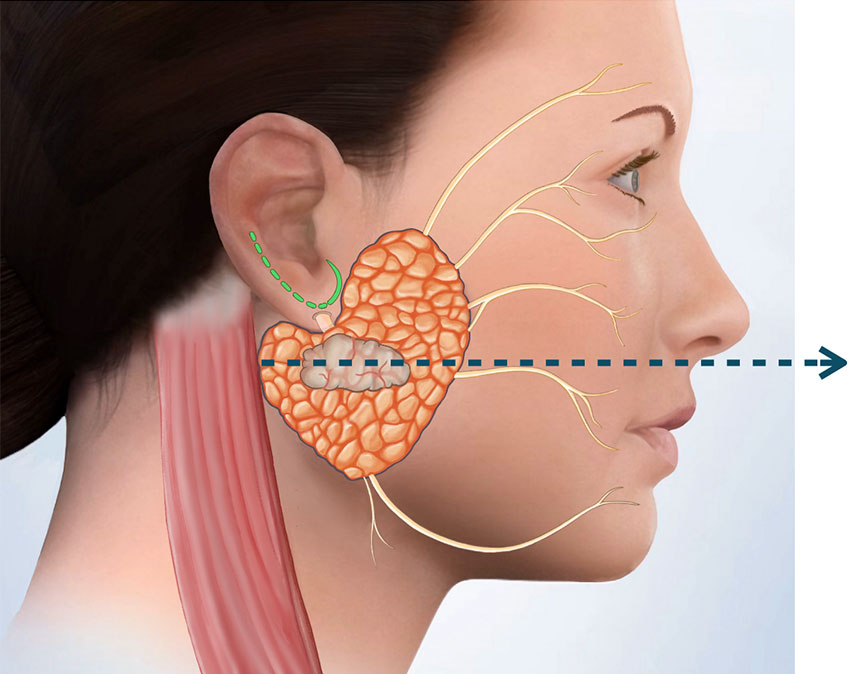
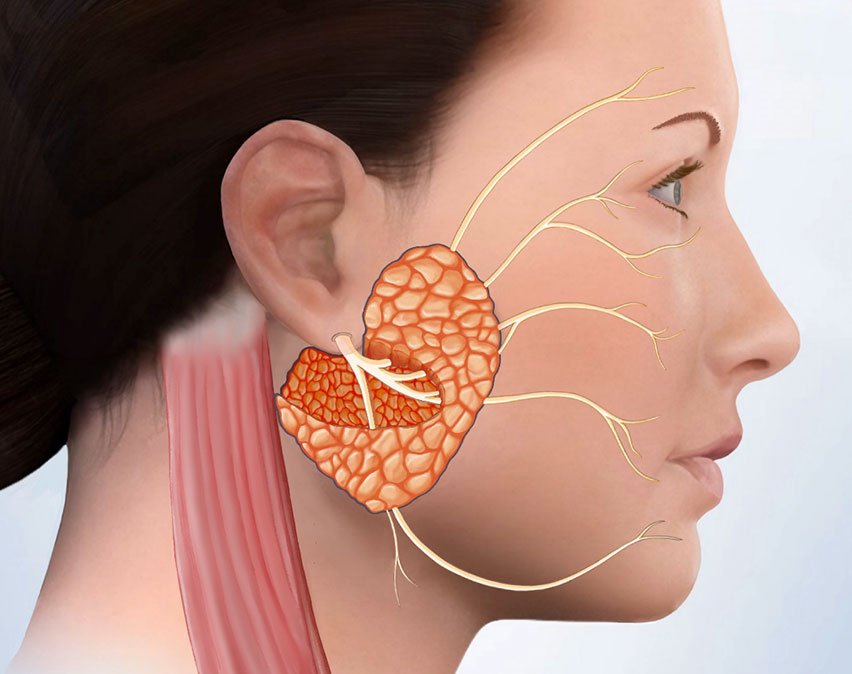
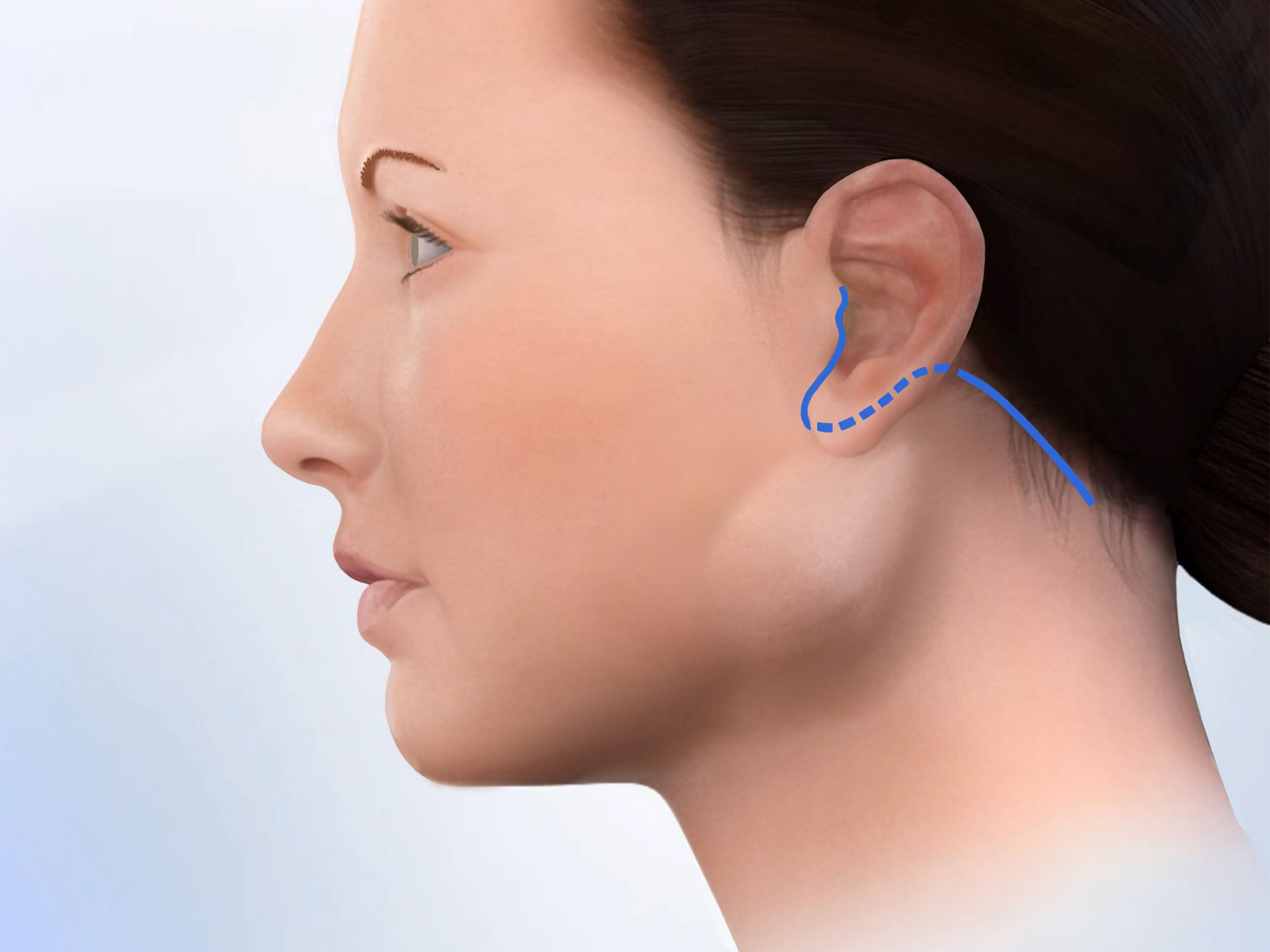
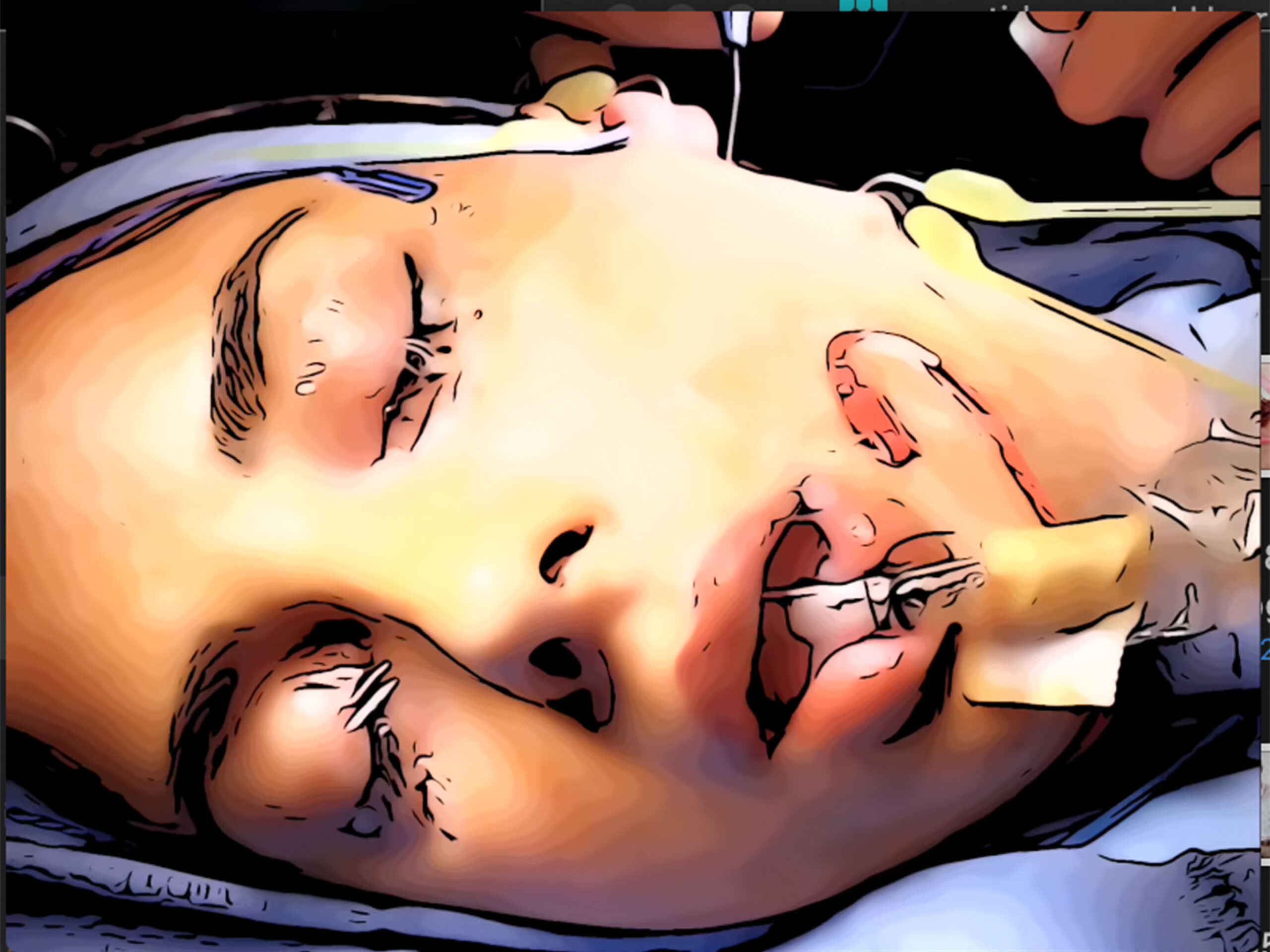
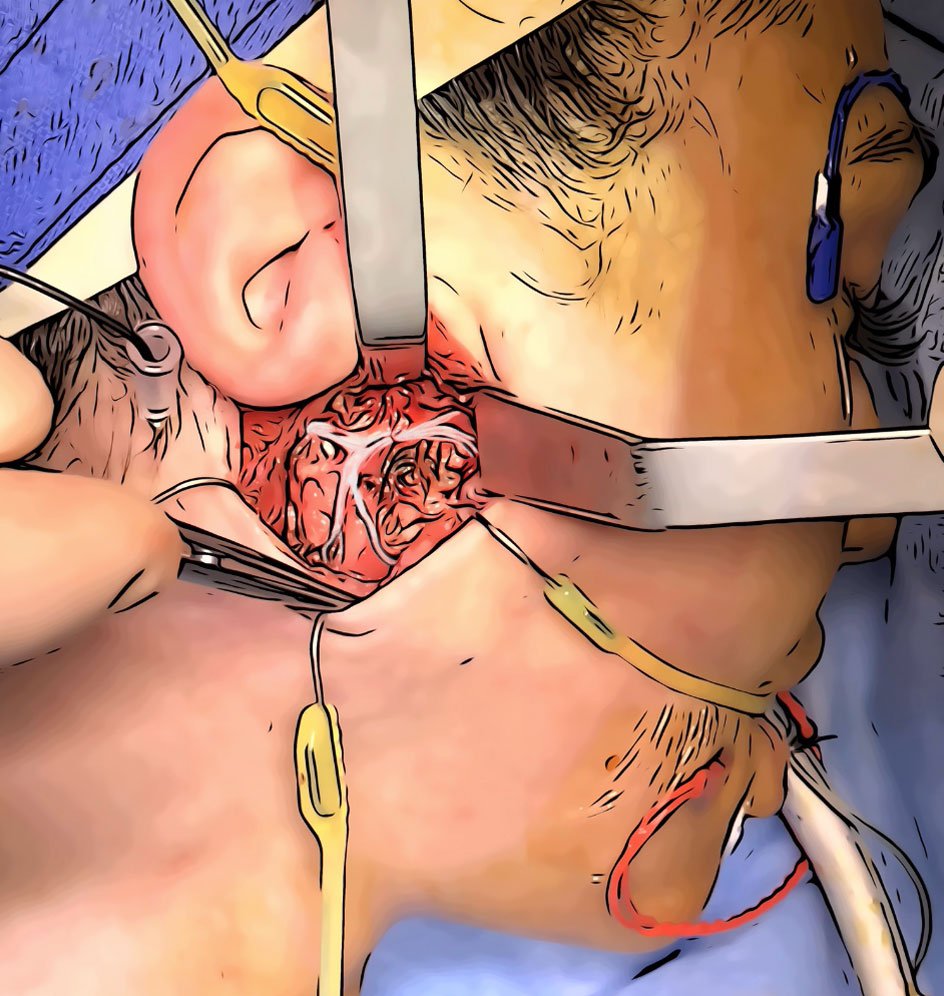
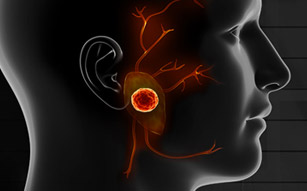
A traditional parotidectomy is performed through a Modified Blair Incision (or lazy S incision). During the procedure, an incision several inches in length is made extending from the top of the ear down toward the jaw. From there, the surgeon is able to visualize the entire side of the face, including the parotid gland, facial nerve, and neck lymph nodes.
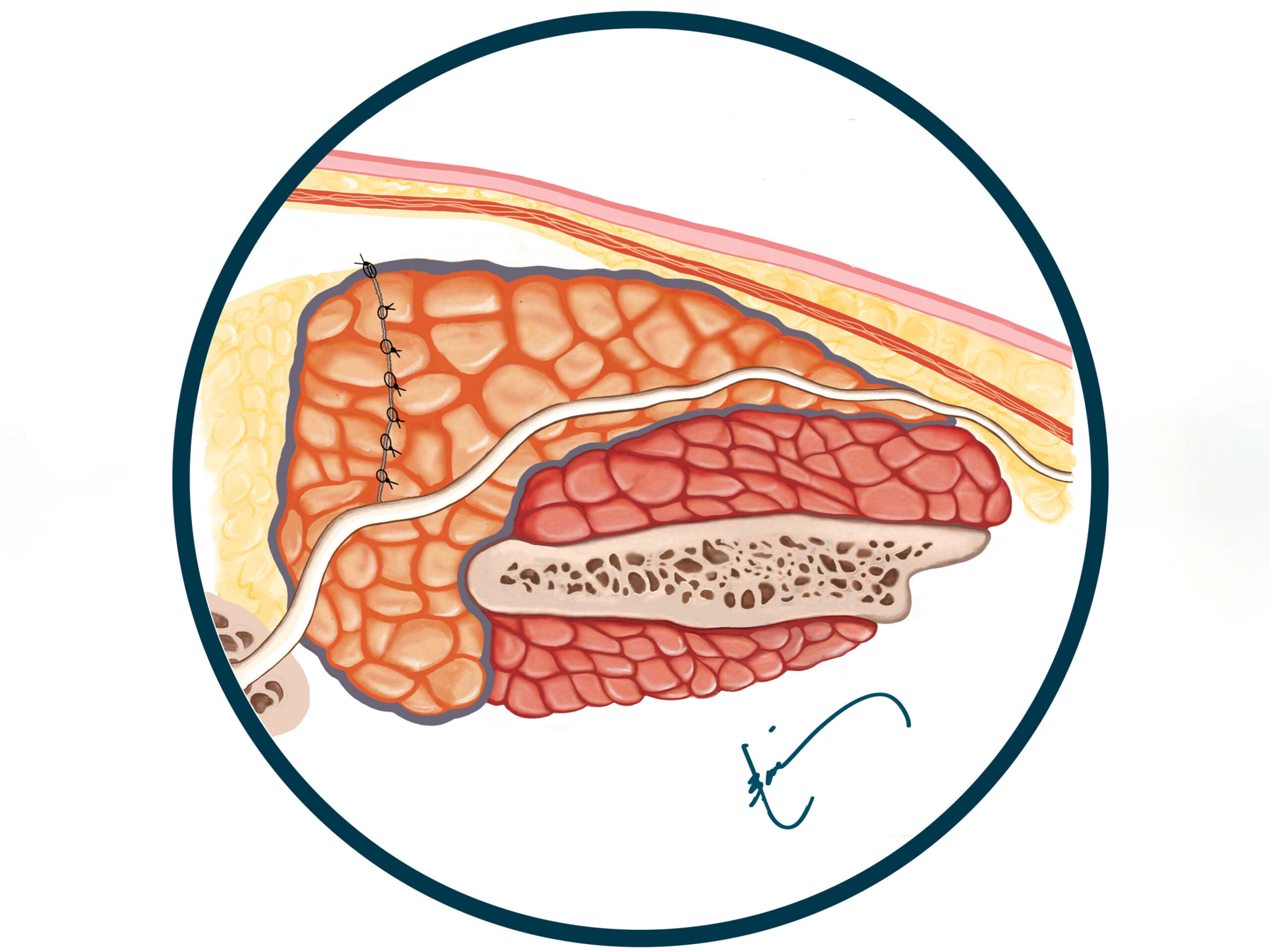
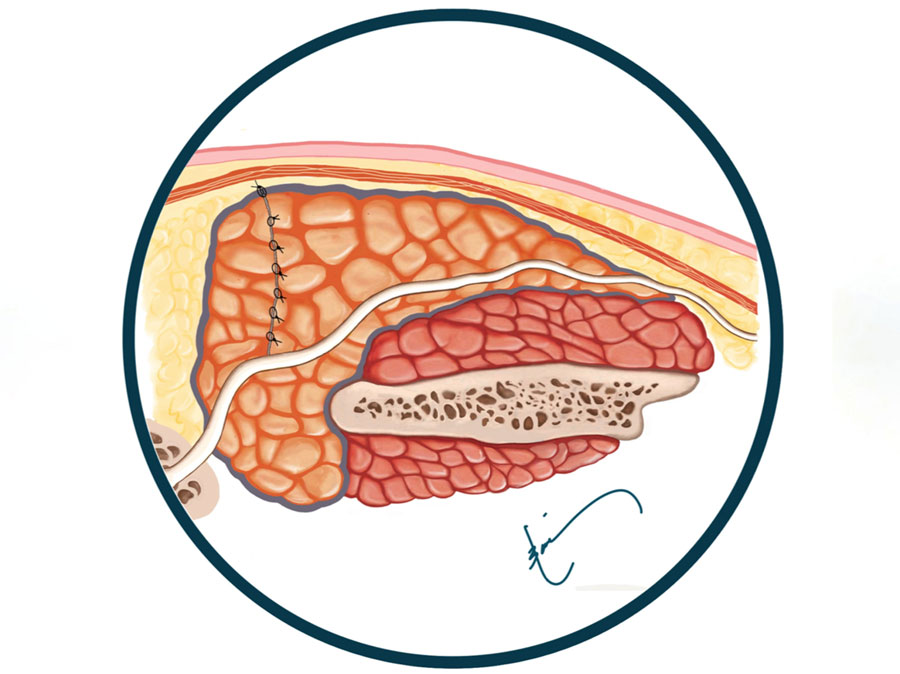
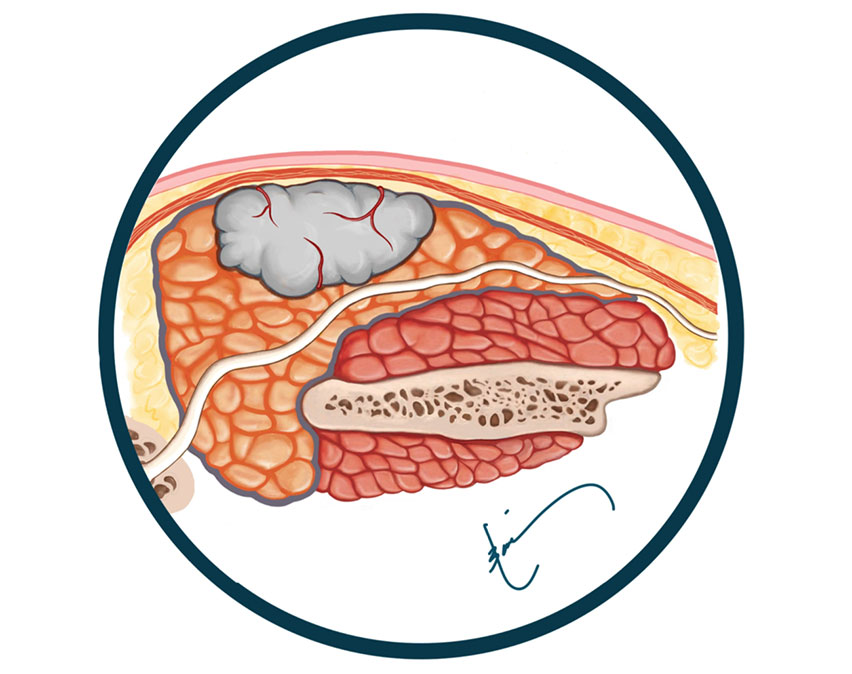
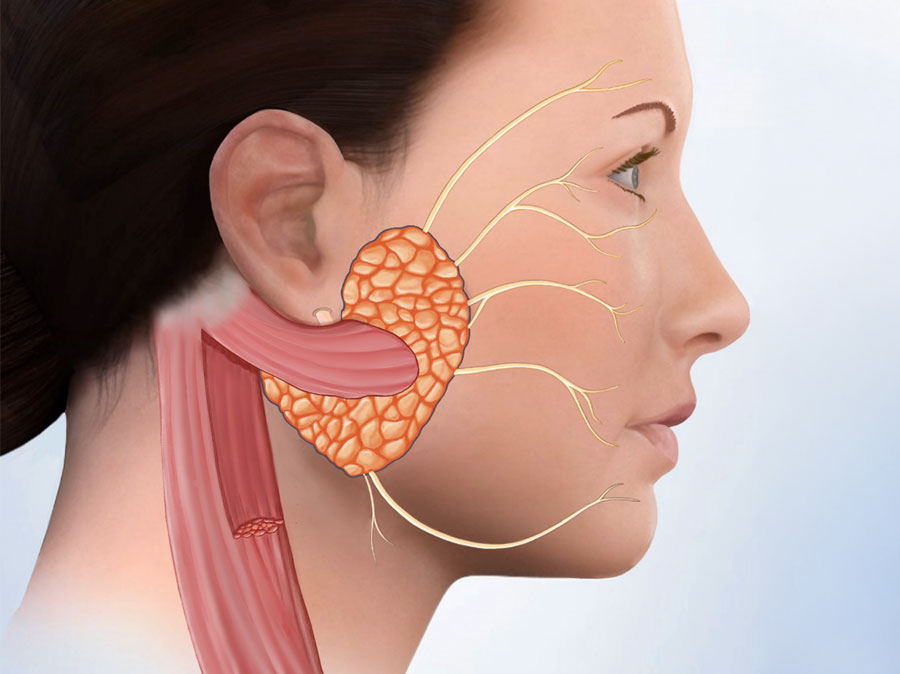
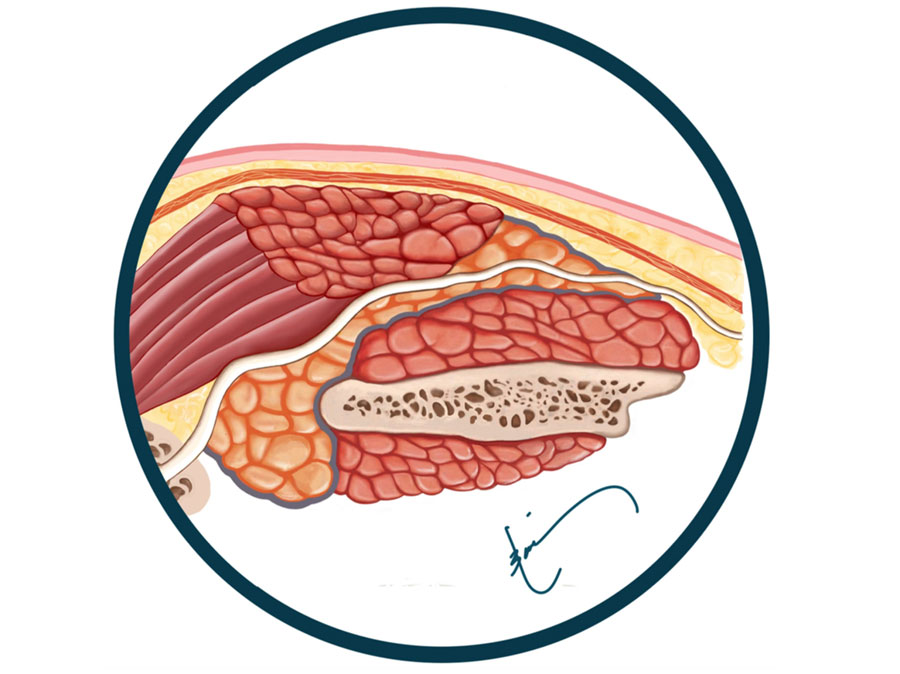
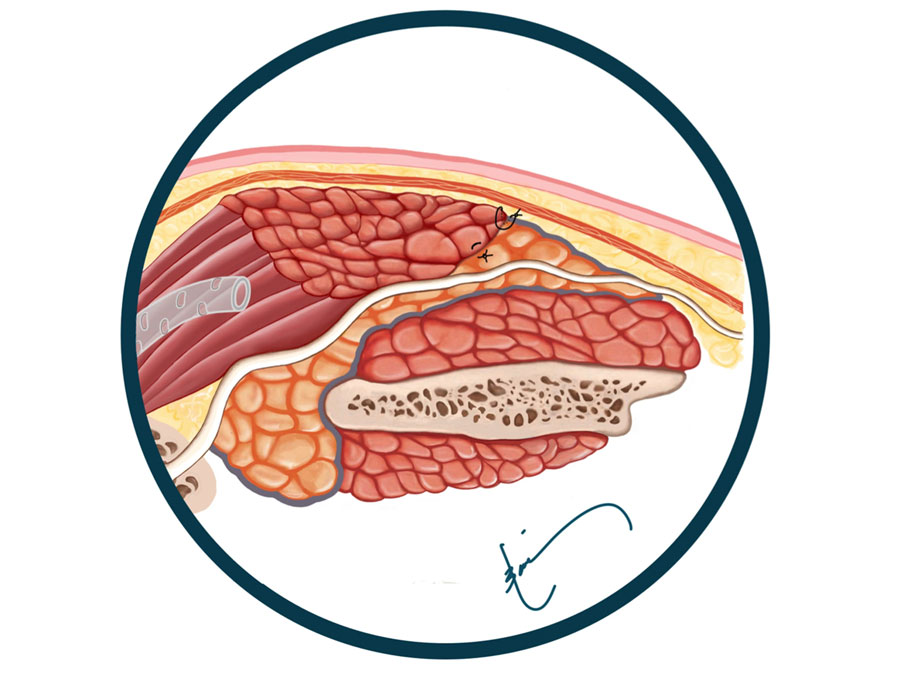
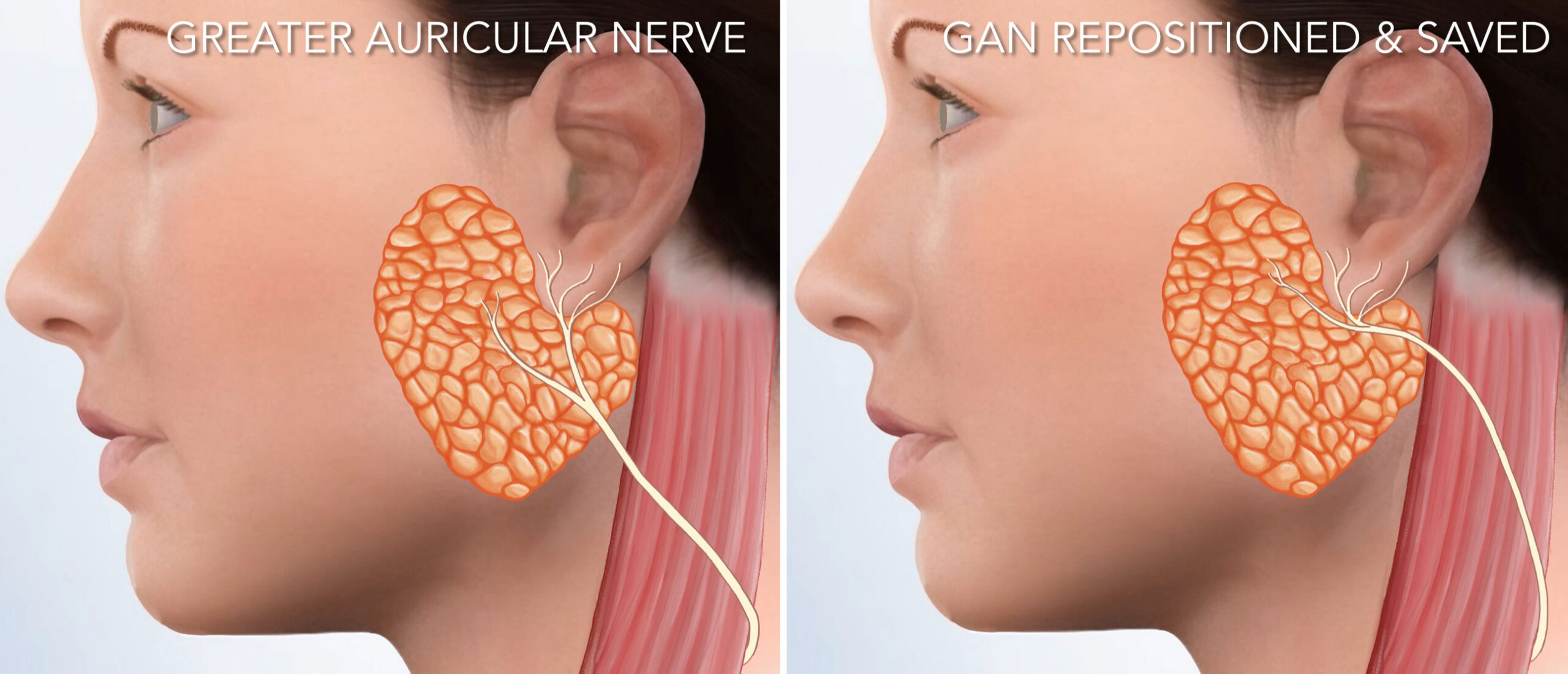
Although this approach is still useful when the removal of lymph nodes is also required, it’s simply not necessary in most cases. Additionally, very few surgeons perform facial reconstruction at the same time as a traditional parotidectomy, leaving patients with a large defect or hollowness in the face & neck where the gland used to be. This also causes most patients to have Frey’s syndrome, which is sweating on the side of the face when hungry or eating (easily preventable by performing a reconstructive surgery at the same time). The traditional surgery also involves cutting the greater auricular nerve, which causes numbness of the lower part of the ear (again this is avoidable).